

World Heart Day: A cardiothoracic surgeon answers questions and clears misconceptions regarding heart transplants
By: Dr Paul Ramesh
Published On: September 29, 2018
On World Heart Day, cardiothoracic surgeon Dr. Paul Ramesh talks about heart transplants and clears all common myths surrounding this procedure.
#DoctorsForGood
Doctors For Good is our community of select, expert doctors from across the country who are working with us to make healthcare accessible to all with the power of crowdfunding. This series is to highlight the day-to-day experiences and bravery of our doctors who are on call to save lives 24x7.
Most of us lead a sedentary lifestyle these days- we spend around 9 hours of our time in front of the desktop and binge on junk food to keep stress at bay. Lack of exercise, proper diet and acute stress has increased the incidences of heart failure in India.

This report talks about the increase in the death rate due to cardiovascular diseases in India by 34% from 115.7 to 209.1 per one lakh population.Heart transplants in India have become fairly common.
However there continue to be doubts as well as misconceptions regarding the procedure. On World Heart Day, we talk to reputed cardiothoracic surgeon Dr. Paul Ramesh, who currently is practicing in Apollo Hospitals Chennai. He explains heart transplant and clears common myths.
 What is a heart transplant?
What is a heart transplant?
Dr Paul Ramesh explains:
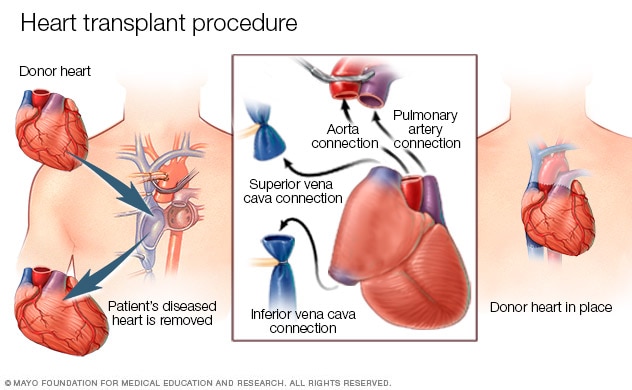
“A heart transplant is essentially a therapy which includes replacing the old heart of the patient with a new heart, from a brain dead donor.
The reasons that you might have to get a transplant is whenever the heart’s pumping ability begins to fail; the pumping efficiency of the heart is a whole spectrum. You may have athletes whose hearts may be able to generate many litres of blood quite easily.
The commonest measure that one uses, which is not very robust, is an echocardiographic called ejection fraction, where you simply put say 100 mls of blood into the heart when its relaxed, and 70 mls, when it’s contracted.
With this procedure, 70 % of the blood should have left the heart. The heart is considered to be healthy when there is 70% functioning of it.
With 50-70% of functioning, is considered to be a moderate impairment in the pumping action and between 30-50% of functioning is severe and below 30% is very severe."
Under what circumstances does a patient need a heart transplant?
First case: Dilated cardiomyopathy
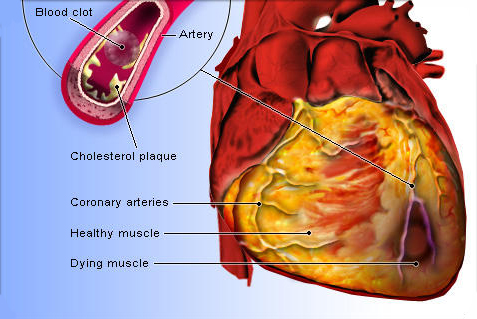
“The muscle of the heart has to be strong and it should have an adequate blood supply, supplied by the artery known as a coronary artery. There are certain diseases that have a genetic basis, and result in a patient suffering from dilated cardiomyopathy, which is the weakening of the heart muscles.
It is an inherent weakness due to some genes that don’t let the heart muscles function in a proper manner. The muscular contraction of the heart is inherently very weak and when the child grows up, they are unable to cope with it and the chambers of the heart begin to dilate, therefore the term dilated cardiomyopathy.”
Second case: Ischemic cardiomyopathy
“The second reason is a similar kind of a situation, not necessarily genetic; because of poor supply of blood to the heart-which can happen in diseases such as hypertension or diabetes- the muscle is weakened over a period of time and it is called ischemic cardiomyopathy.”
Third case: A major heart attack
“Another very common reason to get a heart transplant is when a person has a major heart attack. It is relatively uncommon now as people are able to quickly reach the hospital, and hence a lot of muscle damage is prevented very quickly.
If you want to prevent major abnormalities in the heart and not become a candidate for a heart transplant, it is best to immediately go to a centre when you have chest pain, where you can have a heart attack treated.
 The quicker you get the heart attack treated, the less muscle you will lose. If you begin to lose 40-50% of the muscle around the heart, then the heart won’t be able to pump blood very well, and that could lead to a pumping failure. “
The quicker you get the heart attack treated, the less muscle you will lose. If you begin to lose 40-50% of the muscle around the heart, then the heart won’t be able to pump blood very well, and that could lead to a pumping failure. “
Fourth case: Viral myocarditis
Another condition is when you can have a viral infection or an inflammation where the muscles of the heart are attacked.
There are certain viruses like adenovirus, in which the structure of the virus resembles the structure of the muscle of the heart, and after the virus infection has come and gone, the immune system seems to think that the heart muscle is actually the virus and then continues to attack it.
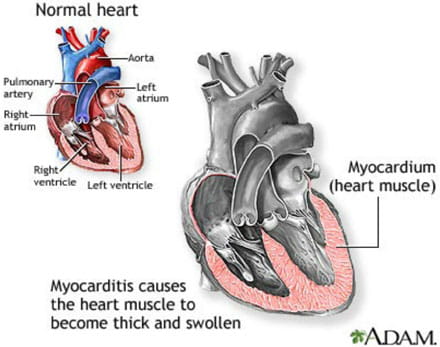
It then becomes viral myocarditis transiting to cardiomyopathy. In all these, the end result is that the muscle of the heart is weakened. But it’s important to note that not everybody with a heart failure needs a heart transplant and not everybody will benefit from it.
Majority of patients, if adequately treated, can lead normal and qualitative lives with a bit of medical management, exercise and diet-most of these things are more than sufficient to keep a person healthy.
Who can get a heart transplant?
“There are three groups of patients for heart transplant:
The first category consists of patients that can live a long and healthy life with some medical management.
 The second category has patients whose health keeps worsening and it needs to be evaluated whether a heart transplant will be useful for them or not.
The second category has patients whose health keeps worsening and it needs to be evaluated whether a heart transplant will be useful for them or not.
In the third category, some of the patients’ heart failure is so advanced that it cause a high pressure in the lungs, which is not reversible and hence it's called irreversible pulmonary hypertension. These patients may not be candidates for a heart transplant.
The major work of a good heart failure unit is to decide which of these categories does a patient belong to.”
What is the procedure to determine whether a patient requires a heart transplant or not?
First step: Detecting the severity of the heart condition

“We do to a four stage assessment, where the first is detecting the severity of the heart condition. We do a right heart cap and a very detailed echocardiography, to detect whether the pulmonary hypertension is reversible or irreversible.
If irreversible, it means that even if I put in a new heart, the lung pressure is not going to come down.
Second step: Combining organ transplants
In the second step, we have to combine the organ transplants in some patients. If some of them have a high pressure in their lungs, we can combine heart and liver transplant, heart and kidney transplant etc.
We have to make sure that the other organs are working well and only a heart transplant alone will be more than sufficient.
Third step: Detecting dormant infections

The third step would be to determine whether there are any dormant infections such bacteria of any kind or whether the person is suffering from TB (Tuberculosis).
This is very important because the moment we transplant a heart, we have to give the patient an immunosuppression where we don’t want any viruses or bacteria to cause a problem. So we screen these patients thoroughly for any dormant infections.
Fourth step: Immunological assessment
The fourth step includes doing an immunological assessment, where we get a reasonable idea on the chances of a patient’s body rejecting the new heart. Some of us, because of childbirth, or various blood transfusions, may have developed antibodies against foreign antigens that can affect the heart.”
What are some of the common misconceptions regarding heart transplants?

“There are a lot of misconceptions regarding a heart transplant, not just amongst the public but amongst doctors too.”
Misconception 1: Heart transplants don’t work
“There is a score system which predicts the mortality of a patient in a year, if he/she doesn’t have a heart transplant. If you take 100 such patients, only 20-30% will be alive, the rest will pass away due to heart failure.
In that subgroup of patients, if your program is delivering 80-90% success rate, then that’s a very good situation. Those patients whose chance of dying within a year is very high, will benefit from a heart transplant, provided that particular unit’s heart transplants outcomes are good.”
Misconception 2: If I have heart failure, I’ll have a heart transplant eventually.
This is not true. Patients can be very stable even after heart failure with proper medicines and vaccines.
Misconception 3: Left ventricular assist devices and heart transplants are competing therapies

“The other misconception is that the left ventricular assist devices and heart transplants are given at equal measures. People think they can either have a ventricular assist device or a heart transplant.
That’s not necessarily true. There are patients that are not qualified for a heart transplant. Some patients may be very old and may not be eligible for a heart transplant for other reasons.
In such cases, we put the ventricular device. In most cases we put the device when there is no heart available and the patient’s health is deteriorating very quickly. So we put the device, make them wait and this procedure is called as a bridge to a heart transplant. These are complementary therapies and not competing therapies.”
Misconception 4: I’ll have to stay in the hospital for a long time after a transplant

“We have had patients who have left the ICU in 3 days and the hospital in 4-5 days with complete mobility.
For our heart failure patients, we make them exercise slowly, to build up their muscle mass. After a lung or a heart transplant, patients get weak very quickly and losing the muscle mass is actually one of the worst things. They can’t breathe very well after the operation as they are super weak.”
Misconception: If I have a heart transplant, I will develop infections
“Yes this can happen but if you take proper care of yourself, take vaccines and keep on doing follow ups, the infection rate can be well controlled.”
What is the status of organ donation in India?
“Organ donation is an absolute must and the awareness has to be increased because I as a doctor can see how sick patients are. They benefit enormously from transplants. As far as the history of transplants is concerned, I have been in the field since 2003, and we have come a long way.
There is better technology now. The perception of transplants is wrong; people tend to think that foreigners are being given preference over Indians for transplants. All that is not true.
I was very surprised as all this did not lead to a reduction rate in organ transplant. A lot of algorithms have been put in place- all patients need to show their Aadhar card, and a proper clearance stating that they have a heart disease.”
We suggest you also read:
The Curious Case Of Benjamin Ward: A Neurosurgeon's Take On Treating Surgery With Depression
Commonly Googled Health Questions Answered By Doctors
If you have any suggestions or feedback related to this article, reach out to us at [email protected]





 Information
Information Alert
Alert