

The Curious Case Of Benjamin Ward: A Neurosurgeon’s Take On Treating Depression With Surgery
By: Dr. PareshDoshi
Published On: August 28, 2018
#DoctorsForGood
Doctors For Good is our community of select, expert doctors from across the country who are working with us to make healthcare accessible to all with the power of crowdfunding. This series is to highlight the day-to-day experiences and bravery of our doctors who are on call to save lives 24x7.
Neurosurgeon Dr. Paresh Doshi talks about his professional journey and the experience of performing a surgery on an Australian suffering from Major Depressive Disorder. Read on!
Dr. Paresh Doshi is a Neurosurgeon, working at Jaslok Hospital in Mumbai. He has 29 years of experience in the field of Neurosurgery.

26-year Australian Benjamin Ward was struck with MDD (Major Depressive Disorder) at the tender age of 21. Talking to anyone seemed like a big task to him and he would frequently be haunted with a desire to kill himself.
When Benjamin first started experiencing depression, he was working at a church-based organization that helped bring about a social change in China. He left his job and returned to America for his medical treatment.
He had tried all treatments possible- medication, shock therapy, psychotherapy etc. but nothing worked. Even antidepressants didn’t work for him.
“People think depression is a feeling, but it is a condition, a disease.”
If there is a history of depression in the family, then the child is likely to suffer from the same. Aside from causing a major sense of despair in a person, Major Depressive Disorder (MDD) causes other issues such as sleep disorders, fatigue, appetite loss and constipation.
Though medication and psychotherapy can cure MDD, there are some patients that don’t recover completely. They are said to suffer from treatment- resistant depression.

In case of Benjamin, Electroconvulsive Therapy ( a procedure conducted under general anesthesia in which small electric currents are passed through the brain, in order to trigger an intentional seizure.
The surgery can cause changes in brain chemistry that can reverse symptoms of certain mental conditions) did help him to some extent but didn’t cure him of his depression fully.
Hence, he was eligible for Deep Brain Stimulation Surgery. (According to Wikipedia, is a neurosurgical procedure involving the implantation of a medical device called a neurostimulator, which sends electrical impulses, through implanted electrodes, to specific targets in the brain for the treatment of movement and neuropsychiatric disorders)
Locating Area 25 in the brain
Benjamin’s uncle and grandfather suffered from depression. Subgenual Cingulate Gyrus or Area 25 of the brain is said to be responsible for causing the same. Area 25 is a vast network in the brain that affects our mood, self-esteem, memory, sleep and appetite.
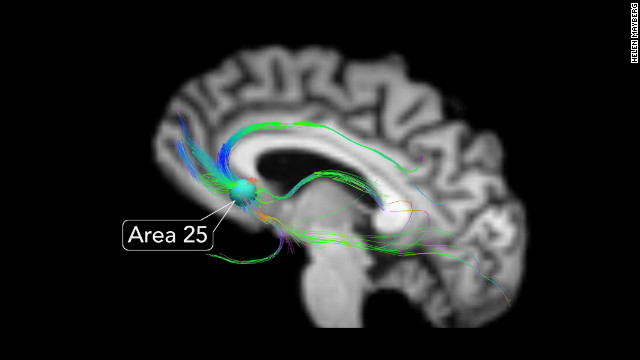
It is found, that in treatment-resistant patients, Area 25 of their brain is overactive, and negative emotions take over positive ones. With DBS surgery (placing electrodes in the white area below Area 25 that stimulates the targeted area), we aimed to cure this and restore positive emotions in Benjamin.
Can Surgery Treat Depression?
There are many controversies and ethical debates surrounding surgeries to treat psychiatric disorders. While some doctors have sworn by DBS and stated that it has helped patients drastically, others have experimented with the surgery and found that not all patients respond well to it.
There is still detailed research required to understand as to why not all patients suffering from MDD, respond to DBS. Some research indicates that while DBS is effective to treat depression, it is not the ultimate cure.
 If the stimulation of the brain stops, the depression will return, which is why it is important for MDD patients to not treat DBS as the final cure, but to keep seeking psychotherapy for continued betterment.
If the stimulation of the brain stops, the depression will return, which is why it is important for MDD patients to not treat DBS as the final cure, but to keep seeking psychotherapy for continued betterment.
Surgical procedures to treat depression were never conducted in India, until 2013, when I became the first surgeon to perform it on Benjamin.
He was on a waiting list in Australia for a DBS surgery but it couldn’t happen due to lack of funds, forcing him to come to India for the procedure.
We had set up a team called the psycho- surgery consensus group in 2009, which came up with guidelines for conducting DBS surgeries in India.Not all patients are considered for the surgery.
A patient for whom all treatment options haven’t worked, can opt for the DBS surgery. The patient is evaluated by an expert team who pass judgement on whether all forms of treatment have been exhausted before or not.
Benjamin gets ready for surgery
Before Benjamin, 29 patients were evaluated but none qualified for the surgery. After a thorough evaluation by neurologists, neurosurgeons, and psychologists, we decided that Ward was the ideal candidate.
On September 25, 2013, Benjamin, who had shaved his head for surgery, was wheeled in. I fixed his head into a rigid stereotactic frame which helped me have a stable reference point, since no two brains are the same.
The surgical procedure: Placing the DBS electrodes
Dr. Paresh Doshi performing DBS surgery on Benjamin. Image credit: The Week
The CT Scans and MRI images helped me visualize Area 25. For the surgery, Benjamin was given local anesthesia and kept fully awake during the procedure. This was done for me to know whether the electrodes had been placed in the correct location, and for this, I needed a confirmation from Ward.
I drilled two holes in the skull through which I inserted the hollow tubes that helped me insert the DBS electrodes. They are tiny and have to be placed in the white matter below Area 25.
Each electrode has four metal pads or contact points, to transmit energy. The current stimulates a tiny part of the brain tissue close to it.
During surgery, we have to find the best contact point to stimulate the targeted area and we do this by asking questions to the patient.
Benjamin’s mental state before and after the surgery
Benjamin smiles for the first time after 5 years during the surgery. Image credit: The Times of India
Before the surgery, I asked Benjamin to rate his sadness from a scale of 1 to 10 and he said, “10 or maybe 8.” I asked him when was the last time he laughed and he said “a long time ago.” I asked Ward if he would like to speak to his best friend and he said “no.”
After the surgery, I kept adjusting the volts of the electrodes, asking him how he was feeling. At one point, he said that he felt lighter, as if the sadness was going away.
When I asked him again if he would like to speak to his best friend, Ward said, “Yup, it would be nice to see him.” It was a sign that he was starting to feel happy. Such conversations would have exhausted him before.
Post the surgery, there was a significant change that we saw in Benjamin. Though he was silent, he appeared to be alert. Even though he spoke in a low voice, he gave us his rare smiles once in a while, and he seemed intrigued by the conversations.
Benjamin with his mother. Image credit: The Week
But, it’s going to take more than one surgery....
However, one surgery is not the answer. It is an ongoing treatment. It is not like appendectomy where you remove an organ and the patient becomes symptom-free. It is like hypertension or diabetes. It has to be managed actively. It does not go away.
Undergoing surgery does not mean that the patient will become happy and chirpy all of a sudden. DBS surgery is primarily responsible for balancing the moods instead of making a patient euphoric. It all depends on the pacemaker; the patient is fine as long as it works.
Benjamin would have to be on continued medication and seek psychiatric help on a regular basis, to get better.
A note on depression
It’s only recently that mental health is beginning to receive the kind of attention that it deserves. Well known personalities such as Deepika Padukone, Selena Gomez, Beyonce etc. have addressed their battles with depression openly, stressing on the fact that depression is not a thought or feeling, but a serious medical condition.
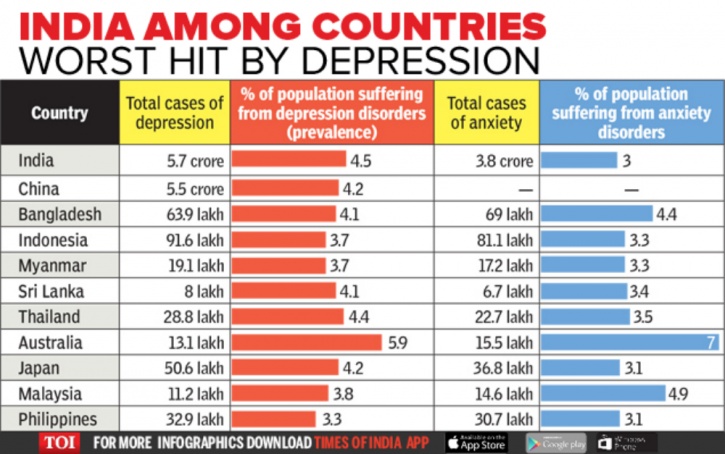
Image credit: IndiaTimes
Clinical depression can be caused by environmental factors such as death of a loved one, work stress, divorce, acute stress, etc. or because of genetics (if someone in your family has suffered from depression).
Aside from this, depression can also be caused by chronic illnesses, prescription drugs, recreational substances such as alcohol and drugs, a head injury, etc.
According to this report, nearly 56,675,969 people in India suffer from depression. 42.5 corporate employees suffer from depression, and 3 of every 100 urban residents in India too suffer from the condition.
Around 1 in 5 people in India either require counselling or psychotherapy. WHO termed India as the world’s most depressed nation.
All these statistics show that depression is an epidemic that requires urgent attention. It has been the cause of several suicides, especially in India.
The topic of depression is still treated as a taboo in India, where many people suffering from it, don’t open up in the fear of being judged as a “psycho” or a “mad person.”
The scenario however needs to change and people need to treat depression as a proper medical condition, just as they treat any other.
We suggest you also read:
National Doctors' Day: 5 Doctors Talk About Saving Lives, Seeing Death And Solving Challenging Cases
If you have any suggestions or questions related to this article, reach out to us at [email protected]








 Information
Information Alert
Alert