Thymoma, a rare type of cancer that originates in the thymus gland, remains a subject of medical intrigue due to its complex nature and diverse manifestations. The thymus, a tiny organ located behind the breastbone and in front of the heart, plays a crucial role in the development and function of the immune system, particularly during childhood. However, as individuals age, the thymus tends to decrease in size and activity, making thymic tumors like thymoma relatively uncommon but significant in clinical practice.
The rarity of thymoma underscores the importance of multidisciplinary collaboration among oncologists, surgeons, radiologists, and other medical professionals to tailor treatment plans according to each patient’s unique clinical scenario. Despite the complexities surrounding thymoma management, advancements in diagnostic techniques, treatment modalities, and supportive care strategies continue to offer hope for patients and caregivers navigating the journey of thymic carcinoma.
Table of Contents
Thymoma Meaning
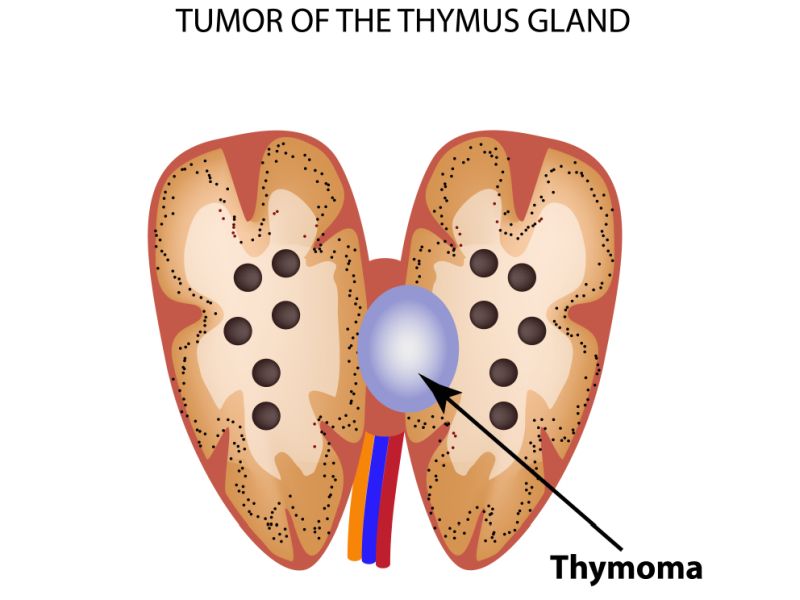
Thymoma is a type of tumor that develops in the thymus gland, which is a small organ situated in the upper chest, just behind the breastbone and in front of the heart. The thymus plays a role in the development of the immune system, particularly in early life. Thymomas emerge from the epithelial cells of the thymus and can vary widely in terms of their behavior and aggressiveness.
Thymic carcinoma, on the other hand, is a type of cancer that also originates from the epithelial cells of the thymus gland. Unlike thymomas, thymic carcinomas tend to be more aggressive & have a higher likelihood of spreading to other parts of the body. They are considered a type of thymic malignancy along with thymomas.
Here are some key differences between thymoma and thymic carcinoma:
1. Behavior and Aggressiveness: Thymomas are generally slow-growing tumors and tend to be less aggressive compared to thymic carcinomas, which are more likely to metastasize to other parts of the body.
2. Histological Features: Thymomas typically have a more well-defined structure and are classified into different subtypes based on their cellular composition, such as type A, AB, B1, B2, and B3 thymomas. Thymic carcinomas often lack this organized structure and are characterized by more aggressive histological features.
3. Prognosis: Thymomas generally have a better prognosis compared to thymic carcinomas. However, the prognosis can differ depending on factors such as the stage of the disease, the subtype of thymoma or thymic carcinoma, and the individual’s overall health.
4. Treatment: Treatment for both thymoma and thymic carcinoma commonly involves surgery to remove the tumor, often followed by other treatments like chemotherapy, radiation therapy, or targeted therapy, based on the stage and characteristics of the tumor.
Individuals with either condition need to work closely with their medical team to decide the most suitable treatment plan based on their specific circumstances. Early detection & intervention can significantly impact the prognosis and outcomes for both thymoma and thymic carcinoma.
Thymoma Symptoms
The symptoms of thymoma can vary depending on factors such as the size & location of the tumor, as well as whether it has spread to other parts of the body. Common symptoms may include:
1. Chest pain: Thymomas can cause discomfort or pain in the chest, which may be persistent or intermittent.
2. Coughing: Chronic coughing or coughing up blood can occur, especially if the tumor is pressing on nearby structures such as the lungs or airways.
3. Difficulty breathing: Thymomas may compress the airways or lungs, leading to shortness of breath or difficulty breathing, particularly during physical activity.
4. Fatigue: Generalized weakness or fatigue can result from the body’s immune system being affected by the tumor.
5. Myasthenia gravis: Thymomas are strongly associated with myasthenia gravis, a neuromuscular illness characterized by muscle weakness & fatigue. Signs of myasthenia gravis may include drooping eyelids, double vision, difficulty swallowing, and weakness in the limbs.
6. Swelling in the face or neck: In some cases, thymomas can cause swelling or enlargement of the face or neck due to pressure on blood vessels or lymph nodes.
7. Weight loss: Unexplained weight loss can occur as a result of the body’s increased metabolic demands or due to the presence of other symptoms, such as loss of appetite.
It’s important to note that thymoma can sometimes be asymptomatic, especially in its early stages, and may be seen incidentally during imaging tests or medical examinations for unrelated conditions. If you experience persistent or concerning symptoms, it’s better to consult with a medical professional for proper evaluation and diagnosis.
Thymoma Treatment
In India, several treatment options are available for managing thymoma and thymic carcinoma. Let’s explore the types of treatments and their costs.
1. Surgery
– Description: Surgery is the most common treatment for early-stage thymoma. It involves removing the tumor & nearby tissue.
– Cost (INR): The cost of thymoma surgery varies based on the hospital, surgeon, and location. On average, it ranges from ₹1,50,000 to ₹3,00,000.
2. Radiation Therapy
– Description: Radiation therapy uses high-energy rays to target cancer cells. It is often used after surgery or as the primary treatment for inoperable cases.
– Cost (INR): The cost of radiation therapy for thymoma typically ranges from ₹1,00,000 to ₹2,50,000.
3. Chemotherapy
– Description: Chemotherapy involves using drugs to kill cancer tumors. It may be administered before or after surgery or as part of a combination treatment.
– Cost (INR): Chemotherapy costs vary widely depending on the drugs used and the treatment duration. On average, it can vary from ₹50,000 to ₹2,00,000 per cycle.
4. Targeted Therapy
– Description: Targeted therapy specifically targets cancer cells without harming healthy cells. It is still being studied and may be available through clinical trials.
– Cost (INR): Costs for targeted therapy can vary significantly. Consult with your oncologist for personalized information.
5. Immunotherapy
– Description: Immunotherapy helps the immune system fight cancer. It is also being explored for thymoma treatment.
– Cost (INR): Immunotherapy costs depend on the specific drugs used and treatment duration. It can range from ₹1,00,000 to ₹3,00,000 per cycle.
6. Hormone Therapy
– Description: Hormone therapy is less common for thymoma but may be considered in certain cases.
– Cost (INR): Costs vary based on the specific hormonal agents used.
7. Clinical Trials
– Description: New treatments are continually being tested in clinical trials. Participation in trials may provide access to cutting-edge therapies.
– Cost (INR): Clinical trial costs are usually covered by the research institution.
Thymoma and thymic carcinoma treatment costs in India can differ based on factors like the stage of the disease, hospital choice, and individual patient needs. It is essential to consult with oncologists & consider all available options to make informed decisions. Remember that timely treatment is crucial for better outcomes.
Thymoma Staging
The most common staging system is the TNM system, which assesses three key factors:
1. Tumor size (T): This describes how far the thymoma has grown into the tissues of the thymus and any nearby structures. Tumor sizes are typically classified as T1 (small) to T4 (larger or more advanced).
2. Lymph node involvement (N): Has the thymoma spread to any lymph nodes? If so, has it affected shallow or deep lymph nodes? N1 denotes that cancer has spread to lymph nodes in the front of your chest, while N2 means it has spread to deeper nodes.
3. Metastasis (M): Has the thymoma spread to organs beyond the thymus, such as the lungs or heart?
The TNM findings determine the stage of your thymoma:
– Stage 1: The thymoma is still contained within the sac around the thymus. It hasn’t deeply invaded surrounding tissues. At this stage, doctors can conduct a surgery called a thymectomy to extract the thymus gland & any affected tissue. The median survival time for anyone with stage 1 thymoma is approximately 166 months (about 14 years), with about 75% living at least 5 years after diagnosis.
– Stage 2: The thymoma has grown beyond the tissues of the thymus and its capsule. It may extend into surrounding fat or the lining of the chest cavity. Symptoms at this stage may include chest pain, pressure, coughing, and difficulty breathing. Treatment options include surgery, chemotherapy, or radiation therapy.
– Stage 3: The cancer has spread further to surrounding body organs like the lungs, sacs around the heart, or large blood vessels.
– Stage 4: Thymomas typically don’t spread beyond the thymus itself; however, any N or M findings usually suggest an advanced (stage 4) thymoma due to their local growth pattern.
Thymoma Causes
While the exact cause of thymoma is not fully understood, various factors may contribute to its development:
1. Genetic Factors: There is proof to suggest that certain genetic mutations or predispositions may increase the risk of developing thymoma. However, specific genetic links to thymoma are still being researched.
2. Autoimmune Disorders: Thymoma is often associated with autoimmune disorders such as myasthenia gravis, where the body’s immune system wrongly attacks its tissues, including the muscles. The thymus plays a role in the development of immune cells, and abnormalities in this process may lead to autoimmune conditions and, in some cases, thymoma.
3. Environmental Factors: While no specific environmental factors have been definitively linked to thymoma, exposure to certain substances or toxins may potentially play a role in its development. However, more research is needed to establish any direct causative relationships.
4. Age and Gender: Thymomas are most commonly detected in adults between the ages of 40 & 60, although they can occur at any age. They are also slightly more common in men than in women.
5. Radiation Exposure: There is some evidence to suggest that exposure to radiation, particularly during childhood or young adulthood, may increase the risk of developing thymoma. However, this association needs to be better understood and requires further investigation.
Overall, the development of thymoma is likely influenced by a combination of genetic, environmental, & immunological factors. However, more research is needed to fully understand the complex mechanisms involved in its pathogenesis.
Thymoma Survival Rate
Survival rates provide an estimate of the likelihood of surviving a specific period after diagnosis. Here are the survival rates for different stages of thymoma:
1) Localized Thymoma (Stage 1):
- Five-Year Relative Survival Rate: Approximately 95%.
- Prognosis: Excellent when the tumor is confined to the thymus gland.
2) Regional Spread (Stage 2):
- Five-Year Relative Survival Rate: Approximately 78%.
- Prognosis: Slightly lower due to regional spread beyond the thymus.
3) Distant Spread (Stage 3):
- Five-Year Relative Survival Rate: Approximately 38%.
- Prognosis: Challenging when the tumor has extensively spread.
Thymoma Diagnosis & Tests
When it comes to diagnosing thymoma, healthcare professionals use a combination of exams and tests to check for signs of this rare cancer. Here are some of the diagnostic methods:
1. Medical History and Physical Exam:
– Your doctor will take a complete medical history and ask about symptoms. They’ll also inquire about your general health.
– During a physical exam, the doctor may feel for any fullness in the lower neck area, which could be associated with thymic cancer.
– Thymomas are often suspected if you have signs and symptoms related to conditions like myasthenia gravis, hypogammaglobulinemia, or red cell aplasia.
2. Imaging Tests:
– These tests create precise images of the inside of your body using X-rays, magnetic fields, or radioactive substances.
Common imaging tests include:
– Chest X-ray: When a problem in the middle of the chest is suspected, a chest X-ray may be the first test recommended. However, some thymomas may not be visible on a chest x-ray.
– Computed Tomography (CT) Scan: Provides detailed cross-sectional images of soft tissues. A chest CT with contrast is often used.
– Magnetic Resonance Imaging (MRI) Scan: Uses radio waves & strong magnets to develop detailed images of soft tissues. Useful for looking at thymus tumors.
– Positron Emission Tomography (PET) Scan: Involves injecting a slightly radioactive form of sugar to detect areas of radioactivity in the body. Helps identify possible cancer spread.
3. Biopsy:
– The only way to positively diagnose thymoma is through a biopsy of the affected tissue.
– A CT-guided needle biopsy can precisely sample the suspected tumor or metastasis.
Remember that early detection & accurate diagnosis are crucial for effective management and treatment of thymoma. If you suspect any symptoms related to this condition, consult a healthcare professional promptly.
Conclusion
In conclusion, thymoma, including thymic carcinoma, presents a complex set of symptoms and treatment challenges. Early detection is crucial for better prognosis, as symptoms may be subtle initially. Treatment options vary based on the stage & severity, ranging from surgery to chemotherapy & radiation therapy. Despite advancements in research and treatment modalities, thymoma remains a rare and often misunderstood condition, emphasizing the importance of continued awareness, research, and multidisciplinary care approaches to improve outcomes for affected individuals.
Thymoma treatment entails various expenses, including surgeries, chemotherapy, radiation therapy, and post-operative care. These costs can quickly accumulate, placing immense strain on patients and their families. A fundraising platform offers a means for individuals to rally support from their social networks, communities, and beyond, easing the financial burden and ensuring access to comprehensive treatment.












