Photodynamic Therapy (PDT) is a cutting-edge medical treatment that harnesses the power of light and photosensitising agents to combat various diseases, including cancer and certain skin conditions. This innovative therapeutic approach integrates principles of chemistry, biology, and physics to achieve targeted and minimally invasive treatment outcomes. PDT holds immense promise in modern medicine, offering a unique combination of precision and selectivity that distinguishes it from conventional treatment modalities.
The roots of Photodynamic Therapy can be dated back to the early 20th century when researchers began finding the phototoxic effects of certain dyes on microorganisms. However, it was in the 1970s that PDT gained substantial attention as a potential medical intervention. The pivotal work of pioneers like Thomas Dougherty and others laid the foundation for understanding the fundamental principles behind PDT. Subsequent advancements in photosensitiser development and light delivery technologies further propelled PDT into the forefront of medical research.
The foremost clinical application of PDT occurred in treating early-stage cancers, particularly dermatology. Since then, PDT has evolved and diversified, finding applications in various medical fields, including oncology, ophthalmology, and dermatology. The continual refinement of PDT protocols and the identification of new photosensitisers have contributed to its expanding role in the therapeutic arsenal against various diseases.
Photodynamic Therapy has emerged as a significant player in modern medicine due to its distinctive features and therapeutic benefits. One of its major benefits lies in its ability to selectively target diseased tissues while sparing healthy surrounding structures. This selectivity minimises collateral damage, making PDT an attractive option for treating conditions where precision is paramount. Furthermore, PDT is a non-invasive or minimally invasive procedure, reducing the associated risks and improving patient outcomes.
As with any medical procedure, the cost of photodynamic therapy (PDT) is a crucial consideration for individuals seeking this innovative treatment. In India, the cost of PDT can differ based on several factors, including the type and stage of the condition being treated, the specific photosensitiser used, the healthcare provider’s expertise, and the treatment facility’s geographical location. Generally, PDT costs in India are relatively competitive compared to many other countries, making it an affordable option for patients seeking advanced medical care without exorbitant expenses.
As the understanding of PDT mechanisms deepens and technology advances, this innovative therapeutic modality is poised to play an increasingly crucial role in the continuum of patient care, representing a beacon of hope for those seeking targeted, effective, and minimally invasive treatments.
Table of Contents
Application Of Photodynamic Therapy (PDT)
Photodynamic Therapy is a medical therapy that uses a photosensitising agent, often a drug or compound activated by light exposure, along with a specific wavelength of light, to treat various medical conditions. The applications of PDT are diverse and can be found in different medical fields.
A. Photodynamic Therapy For Cancer
PDT is a medical treatment that uses special drugs, sometimes called photosensitisers, along with light to damage cancer cells. The drugs only work after they have been “turned on” or activated by certain types of light. PDT may also be referred to as photo radiation therapy, phototherapy, or photochemotherapy.
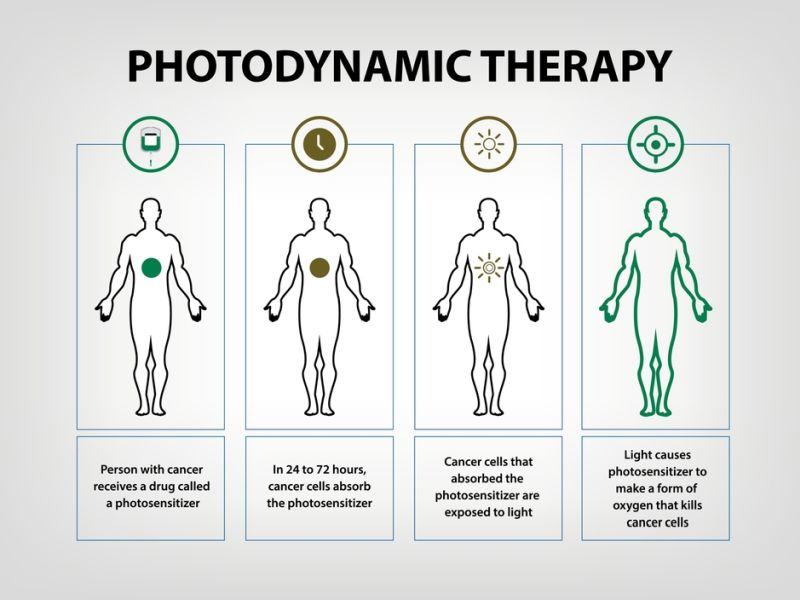
PDT is a two-step process. First, you will receive a photosensitiser. The drug may be consumed by mouth, spread on the skin, or recommended through an IV, based on where the tumour is in the body. After 24 to 72 hours, most drugs will have left normal cells but stay in cancer or precancer cells. Then, your tumour will be exposed to a light source.
How the light is applied depends on where the cancer tumour is. For skin cancer, the light is sought right at cancer. For tumours in the throat, airways, & lungs, your doctor will put an endoscope (An endoscope is a thin, lighted tube that can assist the physician in seeing inside the body) down your throat. Once the endoscope is fixed, the physician knits a fibre optic cable that transmits light to the treatment areas.
When cells that have absorbed photosensitisers are exposed to a specific wavelength of light, the photosensitiser creates a form of oxygen, called an oxygen radical, that kills them. PDT may also influence blood vessels in the tumour, which restricts it from getting the blood it needs to keep growing. It may trigger the immune system to attack tumour cells, even in other areas of the body.
PDT is often used as a local treatment, treating a specific body part. The FDA has approved PDT to treat some skin, lung, and esophageal cancers and precancers. PDT is also used to relieve symptoms of some cancers, such as oesophagal cancer, when it blocks the throat or non-small cell lung cancer or when it blocks the airways.
PDT has some benefits over other cancer treatments. It can target cancer cells while sparing normal cells. It can be repeated many times at the same site if needed. It can be combined with other treatments such as surgery, chemotherapy, or radiation therapy. And it has fewer side effects than some other treatments.
PDT also has some cons. It can only heal areas where light can reach. It cannot treat large or deep tumours. It may cause sensitivity to light for several weeks after treatment. And it may not be covered by some insurance plans.
Some side effects of PDT include skin redness, swelling, pain, burning, or itching at the treatment site; sensitivity to light for up to six weeks after treatment; nausea and vomiting; coughing or trouble breathing; and infection or bleeding at the treatment site. These side effects are usually mild and disappear within a few days or weeks.
B. Dermatology
1. Acne Treatment:
– Mechanism: PDT treats acne by targeting and destroying the sebaceous glands contributing to acne formation. A photosensitising agent is applied to the skin, and the affected areas are exposed to light, reducing oil production and inflammation.
– Advantages:
– Non-Invasive: PDT for acne is a non-invasive alternative to systemic treatments.
– Reduction in Scarring: PDT can help reduce the risk of scarring associated with severe acne.
– Limitations:
– Temporary Redness: Patients may experience temporary redness and sensitivity to light after treatment.
– Multiple Sessions: It might be required for optimal results.
2. Psoriasis and Other Skin Conditions:
– Mechanism: PDT has been explored for treating psoriasis and other skin conditions by targeting abnormal skin cell growth. A photosensitising agent is applied, and affected areas are exposed to light.
– Advantages:
– Localized Treatment: PDT can provide localised treatment for specific skin lesions.
– Reduced Side Effects: Compared to systemic treatments, PDT may have fewer systemic side effects.
– Limitations:
– Limited Depth of Treatment: PDT is limited to superficial skin lesions like in acne treatment.
C. Ophthalmology
1. Macular Degeneration:
– Mechanism: PDT treats age-related macular degeneration (AMD). A photosensitising agent is infused into the bloodstream, and light is applied to the affected area. This helps to close abnormal blood vessels and slow the progression of AMD.
– Advantages:
– Minimally Invasive: PDT for AMD is a minimally invasive procedure.
– Preservation of Vision: It can help preserve central vision by preventing abnormal blood vessel growth.
– Limitations:
– Temporary Vision Changes: Patients may experience temporary changes in vision after treatment.
– Limited Effectiveness: PDT may not be effective for all types of AMD.
2. Glaucoma:
– Mechanism: PDT has been investigated as a potential treatment for certain types of glaucoma. It involves using a photosensitising agent to target the cells responsible for fluid drainage in the eye, thus reducing intraocular pressure.
– Advantages:
– Minimally Invasive: PDT for glaucoma is a minimally invasive option.
– Potential for Lowering Intraocular Pressure: It may sometimes help lower intraocular pressure.
– Limitations:
– Limited Studies: Research on PDT for glaucoma is ongoing, and its efficacy is still being explored.
– Temporary Effects: The effects of PDT on intraocular pressure may be temporary.
In summary, Photodynamic Therapy is a versatile treatment modality with applications in oncology, dermatology, and ophthalmology. While it has shown success in various conditions, ongoing research is essential to refine techniques, broaden applications, and address limitations.
What Is Photodynamic Therapy?
Photodynamic therapy is a medical therapy that combines photosensitising agents, light, and oxygen to destroy abnormal or cancerous cells selectively. This therapy is used to treat various medical conditions, including certain types of cancer and certain non-cancerous conditions.
Here’s how photodynamic therapy generally works:
1. Photosensitizing Agent Administration: Patients are administered a photosensitising drug, which is a substance that makes cells sensitive to light. This drug is often given orally or through injection and is absorbed by cells throughout the body.
2. Accumulation in Target Cells: The photosensitising agent tends to accumulate more in the targeted abnormal or cancerous cells than in normal cells.
3. Light Activation: After a sufficient amount of time has passed to allow the drug to be taken up by the target cells, the area to be treated is exposed to a specific wavelength of light. This light activates the photosensitising agent in the target cells.
4. Production of Reactive Oxygen Species (ROS): When activated by light, the photosensitising agent reacts with oxygen to produce reactive oxygen species (ROS). These ROS are toxic and cause damage to the targeted cells.
5. Cell Destruction: The ROS generated during the process induces cell death in the targeted cells through apoptosis (programmed cell death) or necrosis.
One advantage of photodynamic therapy is its ability to selectively target and destroy abnormal cells, minimising damage to surrounding healthy tissues. However, its effectiveness can differ depending on the treatment condition, the type of photosensitising agent used, and other factors.
Photodynamic Therapy Cost In India
The cost of PDT in India depends on several factors, such as:
– The type and location of the disease or condition being treated.
– The number and duration of PDT sessions required.
– The type and dose of photosensitiser used.
– The type and source of light used.
– The hospital where the treatment is conducted.
– The doctor’s fees and other charges.
The average cost of PDT in India ranges from Rs. 1200 to Rs. 500000 per session. A series of PDT treatments can cost more than Rs. 1000000 over a few months or years. PDT is available in many hospitals and clinics across India with specialised equipment and trained staff. Some of the reputed hospitals that offer PDT in India are:
– Apollo Hospitals
– Medsurge India
– Narayana Superspeciality Hospital
– Sankara Nethralaya
– Memorial Hospitals Group
– KIMS Hospital
– HCG Cancer Centre
You can consult with these hospitals online or offline to learn more about their services, facilities, charges, and availability.
What To Expect Before, During & After Photodynamic Therapy (PDT)?
Before PDT, you will receive photosensitiser, which may be taken by mouth, applied on the skin, or infused into a vein, depending on where the abnormal cells are located. The photosensitiser will make the abnormal cells more sensitive to light, but it will also make your skin and eyes more sensitive to sunlight and bright indoor lights for several days or weeks. You must avoid exposure to direct sunlight & bright lights until the sensitivity wears off.
During PDT, your doctor will use a light source, such as a laser or an LED, to activate the photosensitiser in the abnormal cells. The light source may be applied directly on the skin or through an endoscope (a thin, flexible tube with a light and a camera) inserted into your body. The light will trigger the photosensitiser to produce a form of oxygen that kills the abnormal cells. The treatment may last from a few minutes to an hour, depending on the area’s size and location. You may feel discomfort, burning or pain during the treatment, which can be relieved with painkillers or cooling devices.
After PDT, you must rest and recover for a few days or weeks. You may experience some side effects, such as redness, swelling, blistering, peeling or crusting of the treated skin; soreness or difficulty swallowing if your throat or oesophagus was treated; coughing or shortness of breath if your lungs were treated; or sensitivity to light in your eyes if your eyes were treated. These side effects are usually temporary & can be handled with medications or wound care. You will also need to follow your doctor’s instructions on protecting your skin and eyes from light exposure until the sensitivity disappears.
Side Effects Of Photodynamic Therapy
While PDT can be effective, it may also be associated with side effects. It’s vital to note that the severity & occurrence of these side effects can differ from person to person. Here are some potential side effects of photodynamic therapy:
1. Skin reactions: Redness, swelling, and a sunburn-like reaction are common side effects. The treated area may be light-sensitive for some time after the procedure.
2. Pain or discomfort: Some people may experience pain or discomfort during or after the light exposure. This can often be managed with pain relievers.
3. Scarring: In some cases, PDT may cause scarring, particularly when treating certain skin conditions or pre-cancerous lesions.
4. Crusting or peeling: The treated skin may develop crusts or peel off. This is a normal part of the healing process, but it’s vital to follow post-treatment care instructions provided by the healthcare provider.
5. Swelling: Swelling may occur in the treated area and usually resolves on its own over time.
6. Hyperpigmentation or hypopigmentation: Changes in skin pigmentation may occur, leading to darkening or lightening of the treated skin. These changes are usually for a limited period but can be permanent in some cases.
7. Infection: While uncommon, there is a risk of infection at the treatment site. It’s essential to follow proper wound care instructions to minimise this risk.
8. Eye sensitivity: If the eyes are exposed to the treatment light, it can cause sensitivity to light (photosensitivity) for a period after the procedure. Protective measures are usually taken to minimise the risk of eye exposure.
9. Allergic reactions: Some individuals may be allergic to the photosensitising agent used in PDT. Allergic reactions can differ from mild to serious, including itching, redness, or hives.
10. Nausea and vomiting: Systemic photosensitisers used in certain types of PDT, especially for internal conditions, may cause nausea and vomiting.
It’s better to discuss potential side effects and risks with your healthcare provider before undergoing photodynamic therapy. They will provide information specific to your condition and help you make an informed decision about the treatment. If you experience severe or persistent side effects, it’s essential to contact your medical provider promptly.
Benefits Of Photodynamic Therapy
Here are some benefits of photodynamic therapy:
1. Cancer Treatment:
– Non-Invasive: PDT is a minimally invasive treatment for certain kinds of cancer, like skin cancer and certain cancers of the oesophagus and lungs. It can be used as an alternative to surgery or radiation therapy in some cases.
– Targeted Treatment: PDT can selectively target cancer cells while minimising damage to surrounding healthy tissues. This targeted approach can help limit side effects compared to traditional treatments.
2. Skin Conditions:
– Acne Treatment: PDT has been used to treat severe cases of acne. The light activates a photosensitising agent applied to the skin, which helps kill acne-causing bacteria and reduce inflammation.
– Actinic Keratosis: PDT effectively treats precancerous skin lesions known as actinic keratosis. It helps eliminate abnormal cells on the skin’s surface.
3. Minimizing Scarring:
– Scar Reduction: PDT has been explored for its potential in reducing scarring, particularly in hypertrophic scars and keloids. By targeting abnormal collagen production, PDT may help improve the appearance of scars.
4. Treatment of Eye Conditions:
– Macular Degeneration: PDT treats certain eye conditions, including age-related macular degeneration (AMD). In this case, PDT helps to close abnormal blood vessels in the retina that contribute to vision loss.
5. Antimicrobial Properties:
– Infections: PDT has antimicrobial properties and has been investigated for treating bacterial and fungal infections. When activated by light, the photosensitising agent can destroy or inhibit the growth of microorganisms.
6. Pain Management:
– Pain Relief: PDT has been explored for its potential in managing pain, particularly in conditions like arthritis. The treatment may help reduce inflammation and alleviate pain symptoms.
7. Cosmetic Applications:
– Skin Rejuvenation: PDT is sometimes used in cosmetic dermatology for skin rejuvenation. It can enrich skin texture, reduce the appearance of fine lines and wrinkles, & enhance overall skin tone.
It’s important to note that while PDT offers several benefits, its applicability depends on the specific condition being treated and individual patient factors.
Emerging Technologies In Photodynamic Therapy (PDT)
One of the challenges of PDT is to deliver light-sensitive drugs, also known as photosensitisers, to the target cells without affecting the surrounding healthy tissue. To overcome this challenge, researchers are developing nanotechnology-based approaches that can enhance the specificity and efficiency of PDT.
1. Nanotechnology in PDT
Nanotechnology is the science & engineering of materials at the nanoscale, which is approx 1 to 100 nanometers in size. Nanomaterials have unique physical & chemical properties that can be exploited for various applications, including PDT. For example, nanoparticles can be used as carriers for photosensitisers, improving their solubility, stability, and biodistribution. Nanoparticles can also be designed to respond to external stimuli, such as light, heat, or pH, and release the photosensitisers on demand. Moreover, nanoparticles can act as light sources themselves, generating reactive oxygen species (ROS) that can damage the target cells.
2. Targeted Drug Delivery Systems
Another way to improve the selectivity and efficacy of PDT is to use targeted drug delivery systems that can recognise and bind to specific receptors or markers on the surface of the target cells. These systems can be based on biological molecules, such as antibodies, peptides, or aptamers, or synthetic polymers, such as liposomes, micelles, or dendrimers. Targeted drug delivery systems can enhance the accumulation and retention of photosensitisers in the target cells, reducing the systemic toxicity and side effects of PDT.
Conclusion
Photodynamic Therapy (PDT) emerges as a promising medical intervention that utilises light-sensitive drugs and specific wavelengths of light to treat various medical conditions. Its multifaceted applications range from dermatology to oncology, showcasing its versatility in addressing different health concerns.
The cost of Photodynamic Therapy in India can fluctuate based on factors like the type and extent of the condition being treated, the choice of photosensitising agent, and the specific medical facility providing the treatment. Patients should be aware of these factors & engage in open discussions with medical providers to gain a complete understanding of the financial elements involved.
In conclusion, Photodynamic Therapy represents a noteworthy advancement in medical science, offering a targeted and less invasive alternative for the treatment of various conditions. Its evolving applications and ongoing research continue to expand its potential, making it an important consideration in the spectrum of available medical interventions. As with any medical decision, individuals are advised to consult with healthcare professionals to determine the most appropriate course of action for their specific health needs.
Medical expenses can quickly accumulate, and PDT is no exception. From diagnosis to treatment sessions, the financial burden can become overwhelming, leading some individuals to forego or delay the therapy they desperately need. A fundraising platform allows patients to reach out to a wider community for financial assistance, reducing the burden on their own resources.












