Myelofibrosis is a rare but severe bone marrow disorder that falls under the umbrella of myeloproliferative neoplasms (MPNs). Characterized by the unusual proliferation of bone marrow cells and the subsequent formation of scar tissue within the marrow, myelofibrosis disrupts the normal blood cell production process. This condition primarily affects the production of red blood cells, causing various symptoms & complications that can significantly influence a person’s quality of life.
Understanding myelofibrosis involves grasping its complex interplay of genetic and environmental factors, recognizing its diverse symptoms, and navigating the available diagnostic and treatment options. As ongoing research continues to shed light on the underlying mechanisms of this disorder, healthcare professionals are better equipped to tailor interventions that can improve the prognosis & overall well-being of individuals affected by myelofibrosis.
Table of Contents
Myelofibrosis Meaning
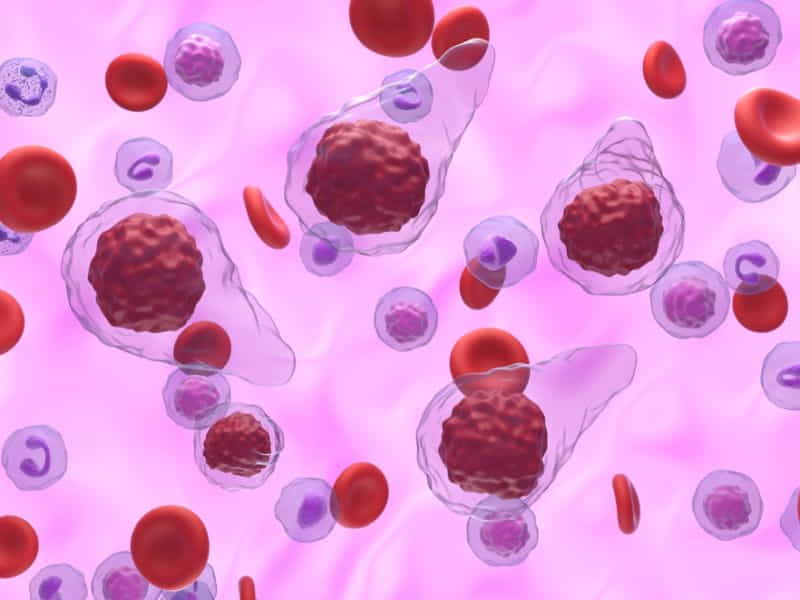
Myelofibrosis is a long-term problem with the bone marrow where fibrous tissue gradually builds up. The bone marrow is the soft part inside our bones that makes blood cells like red and white blood cells. In myelofibrosis, too much fibrous tissue forms in the bone marrow, affecting its normal function.
In myelofibrosis, the normal bone marrow tissue is gradually replaced by scar tissue (fibrosis). This fibrosis disrupts the normal production of blood cells, leading to various complications. Myelofibrosis is considered one of the Philadelphia chromosome-negative myeloproliferative neoplasms, a group of disorders characterized by the overproduction of blood cells.
Myelofibrosis Treatment
There is no cure for myelofibrosis, but treatments can help handle the symptoms & improve the quality of life of people with this disease. The treatment options depend on various factors, like the severity of the symptoms, the risk category of the disease, the presence of gene mutations, and the person’s overall health.
Some people with mild or no symptoms may not need treatment right away. They may only require regular monitoring and supportive care, such as blood transfusions, iron supplements, or antibiotics. Others with more severe or high-risk myelofibrosis may benefit from more aggressive treatments, such as:
– Medications: Different types of drugs can help reduce the symptoms and complications of myelofibrosis. Some examples are:
– Ruxolitinib: This kinase inhibitor blocks a protein called JAK2, which is involved in the abnormal growth of blood cells. Ruxolitinib can reduce the size of the spleen and improve the quality of life of people with myelofibrosis. It is approved for people with intermediate or high-risk myelofibrosis who have a JAK2 mutation or not.
– Thalidomide, lenalidomide, and pomalidomide: These are immunomodulators that can boost the immune system and affect the growth of blood cells. They can improve blood counts and shrink the spleen in some people with myelofibrosis. They are usually used in combination with steroids or other drugs.
– Hydroxyurea: This chemotherapy drug can lower the number of white blood cells and platelets in people with myelofibrosis. It can help prevent bleeding and infection complications and reduce the spleen size.
– Epoetin alfa and darbepoetin alfa: These are synthetic forms of erythropoietin, a hormone that stimulates the production of red blood cells. They can help treat anemia in some people with myelofibrosis.
– Splenectomy: This is a surgery used to remove the spleen, which can become very large and cause pain, discomfort, and early satiety in people with myelofibrosis. Splenectomy can also improve the blood counts and reduce the need for transfusions. However, it also increases the risk of infection and bleeding, so it is usually reserved for people who do not respond to other treatments or have severe symptoms.
– Radiation therapy: This treatment uses high-energy beams to kill cancer cells or shrink tumors. It can decrease the size of the spleen or other organs affected by myelofibrosis. It can also help relieve bone pain or bleeding problems.
– Stem cell transplant: This procedure replaces the damaged bone marrow with stem cells from a fit donor. It is the only medical treatment that can potentially cure myelofibrosis or significantly prolong survival. However, it is also a very risky and complex procedure that requires intensive preparation and follow-up care. It is only suitable for people who are young, healthy, and have a compatible donor.
The choice of treatment for myelofibrosis depends on each individual’s situation and preferences. It is better to discuss the benefits & risks of each option with your doctor and make an informed decision together.
Types Of Myelofibrosis
Myelofibrosis is a rare kind of chronic leukemia characterized by the proliferation of unusual bone marrow cells that replace healthy bone marrow with fibrous scar tissue. This medical condition falls under the category of myeloproliferative neoplasms (MPNs), a group of disorders involving the unusual growth of blood cells in the bone marrow. Myelofibrosis can be classified into different types based on various factors, including its progression and underlying genetic mutations. The two main types are primary myelofibrosis (PMF) and secondary myelofibrosis.
1. Primary Myelofibrosis (PMF):
– Definition: PMF is also known as chronic idiopathic myelofibrosis or agnogenic myeloid metaplasia. It is considered a primary disorder that arises without a known cause.
– Symptoms: Patients with PMF may experience fatigue, weakness, enlarged spleen and liver, anemia, easy bruising, and increased susceptibility to infections.
– Pathophysiology: PMF is characterized by the clonal proliferation of abnormal megakaryocytes (a type of blood cell precursor) in the bone marrow. This leads to the release of fibrogenic cytokines, which stimulate the production of fibrous tissue, resulting in bone marrow fibrosis.
2. Secondary Myelofibrosis:
– Definition: Secondary myelofibrosis is a condition in which fibrosis develops due to other pre-existing hematologic disorders. It is also known as post-polycythemia vera myelofibrosis (PPV-MF) or post-essential thrombocythemia myelofibrosis (PET-MF).
– Causes: It often arises as a progression from other MPNs, such as polycythemia vera or essential thrombocythemia. Over time, these conditions may transform into myelofibrosis.
– Symptoms: Similar to PMF, patients with secondary myelofibrosis may experience symptoms such as fatigue, enlarged spleen and liver, anemia, and other complications associated with bone marrow dysfunction.
3. Other Classifications:
– Prefibrotic Myelofibrosis: Some patients may initially present with a pre-fibrotic stage characterized by significant bone marrow fibrosis but without the classic clinical symptoms of myelofibrosis.
– Post-essential thrombocythemia Myelofibrosis (PET-MF) and Post-Polycythemia Vera Myelofibrosis (PPV-MF): These terms specifically describe myelofibrosis that develops as a progression from essential thrombocythemia or polycythemia vera, respectively.
4. Genetic Mutations:
– It is associated with various genetic mutations, including mutations in genes like JAK2, CALR, and MPL. These mutations play a role in the dysregulation of signaling pathways that control the production of blood cells.
It’s important to note that the classification and understanding of myelofibrosis continue to evolve with ongoing research and advancements in molecular biology. Patients with myelofibrosis often require close monitoring and individualized treatment plans based on their specific circumstances.
Causes Of Myelofibrosis
The exact cause of myelofibrosis is not fully understood, but it is believed to result from genetic mutations in the bone marrow cells, leading to abnormal growth and functioning of these cells. Here are some factors associated with the development of myelofibrosis:
1. Genetic Mutations: It is often associated with specific gene mutations that regulate the production and functioning of blood cells. Mutations in genes like JAK2, CALR, and MPL are commonly found in individuals with myelofibrosis. These mutations lead to the abnormal proliferation of bone marrow cells.
2. Age: Myelofibrosis is more common in older people, with the majority of cases diagnosed in individuals over the age of 50. However, it can occur at any age.
3. Previous Blood Disorders: Some cases of myelofibrosis may arise as a progression from other myeloproliferative disorders, like polycythemia vera or essential thrombocythemia.
4. Exposure to Radiation: Some evidence suggests that exposure to high levels of ionizing radiation may increase the risk of developing this rare disease. This is more relevant in cases of radiation therapy for other cancers.
5. Chemical Exposure: Prolonged exposure to some chemicals, like benzene, has been linked to an increased risk of getting myelofibrosis.
6. Inflammatory Conditions: Chronic inflammation may contribute to the development of myelofibrosis. In some cases, inflammation in the bone marrow can trigger the abnormal growth of cells.
7. Unknown Factors: In some cases, the cause of myelofibrosis remains unknown. There may be a combination of genetic & environmental factors that contribute to the development of the disease.
Myelofibrosis Life Expectancy
Life expectancy can also differ based on the type and stage of a disease. Some diseases are more aggressive and have a worse prognosis than others. Some diseases can be cured or controlled with treatment, while others may not respond well to available therapies.
Myelofibrosis is one of the diseases that can affect life expectancy significantly. According to various studies, the median survival of patients with myelofibrosis is 3.5-5.5 years, & the 5-year survival is reduced to about half of what is expected for that appropriate age group and sex. Approximately <20% of patients survive for 10 years.
However, these numbers are only averages and do not reflect each patient’s individual situation. Some of the factors that can affect the life expectancy of someone with myelofibrosis are:
– Age: Older patients tend to survive shorter than younger patients.
– Blood cell counts: Low levels of red blood cells (anemia), white blood cells (leukopenia), or platelets (thrombocytopenia) can indicate a more advanced disease and a poorer outcome.
– Symptoms: The presence & severity of symptoms such as fatigue, night sweats, fever, bone pain, or spleen enlargement can affect the quality of life and the response to treatment.
– Gene mutations: Certain gene mutations, such as JAK2, CALR, or MPL, can be associated with myelofibrosis. These mutations can affect the disease behavior and the response to treatment differently. For example, JAK2 mutation is linked to a higher risk of blood clots and a lower response to certain drugs.
– Treatment: The type & effectiveness of treatment can also influence the life expectancy of someone with myelofibrosis. There is no cure for this rare disorder, but there are medical therapies that can help manage the symptoms & complications of the disease. These include blood transfusions, drugs that reduce inflammation or inhibit abnormal cell growth (such as ruxolitinib), chemotherapy, radiation therapy, hormone therapy, or stem cell transplantation. The choice and outcome of treatment depend on many factors, such as the patient’s age, general health, disease stage, and personal preferences.
Therefore, it is crucial to understand that life expectancy is not a definite prediction but rather an estimate based on statistics and probabilities. Each patient with myelofibrosis has a unique situation that may differ from the average. The best way to know more about your specific prognosis and treatment options is to talk to your doctor or hematologist-oncologist (a specialist in blood cancers). They can offer more personalized information & guidance based on your medical history, test results, and goals.
Myelofibrosis Symptoms
The symptoms of myelofibrosis can differ from person to person, & some individuals may not experience noticeable symptoms. Common symptoms include:
1. Fatigue: People with myelofibrosis often experience fatigue & weakness due to a reduced number of healthy blood cells, including red blood cells, responsible for carrying oxygen to the body’s tissues.
2. Shortness of Breath: Anemia resulting from the decreased production of red blood cells can cause reduced oxygen-carrying capacity, causing shortness of breath and difficulty breathing.
3. Enlarged Spleen (Splenomegaly): The abnormal production and accumulation of blood cells in the bone marrow can cause the spleen to become enlarged. An enlarged spleen can cause discomfort or a feeling of fullness in the abdomen.
4. Unexplained Weight Loss: Some individuals with this rare disease may experience unintentional weight loss.
5. Bone Pain or Joint Pain: The unusual proliferation of fibrous tissue can cause joint pain in the bone marrow.
6. Easy Bruising and Bleeding: It can reduce the number of platelets (blood cells responsible for clotting), increasing the risk of easy bruising and bleeding.
7. Night Sweats: Some individuals may experience night sweats, which can be disruptive to sleep.
8. Fever: Individuals with this rare disorder may occasionally have an elevated body temperature.
Myelofibrosis Treatment Cost In India
The cost of myelofibrosis treatment in India depends on several factors, such as:
– The type and stage of the disease
– The choice of treatment and hospital
– The duration and frequency of treatment
– The availability of insurance or financial assistance
– The exchange rate of INR to other currencies
The average cost of myelofibrosis treatment in India ranges from INR 5 lakhs to INR 20 lakhs (approximately USD 6,700 to USD 26,800). This may include the cost of consultation, medication, transfusion, surgery, radiation therapy, or bone marrow transplant. However, this is only an estimate and may vary depending on the individual case and circumstances.
The cost of myelofibrosis treatment in India varies depending on the type of treatment, the hospital, the doctor, and the patient’s condition. The approximate costs of some of the treatments are:
| Myelofibrosis Treatment | Cost In India |
| ASCT | Rs. 25-30 lakhs ($32,000-$38,000) |
| Ruxolitinib | Rs. 1.5-2 lakhs ($1,900-$2,600) per month |
| Hydroxyurea | Rs. 500-1000 ($6-$13) per month |
| Splenectomy | Rs. 2-3 lakhs ($2,600-$3,900) |
| Splenic irradiation | Rs. 50,000-1 lakh ($650-$1,300) |
| Blood transfusions | Rs. 5,000-10,000 ($65-$130) per unit |
| Medications | Rs. 1,000-5,000 ($13-$65) per month |
These costs are only indicative and may vary depending on various factors. It is advisable to consult a doctor and a hospital for the exact cost of myelofibrosis treatment in India. Some of the top hospitals for myelofibrosis treatment in India are:
– Gleneagles Global Hospitals
– BLK Super Speciality Hospital
– Tata Memorial Hospital
– Apollo Hospitals
– Fortis Hospital
Risk Factors Of Myelofibrosis
While the exact cause of myelofibrosis is often unknown, there are certain risk factors & potential contributing factors associated with the development of this condition. It is important to remember that having one or more risk factors does not guarantee the development of myelofibrosis, and some people with the condition may not have any known risk factors.
Here are some recognized risk factors and contributing factors:
1. Age: It is more commonly diagnosed in individuals over 50, and the risk increases with age.
2. Gender: It appears that it affects men and women equally, although some studies suggest a slightly higher prevalence in men.
3. Genetic Mutations: Genetic mutations have been associated with myelofibrosis, including mutations in the JAK2, CALR, and MPL genes. These mutations are found in a significant percentage of people with myelofibrosis.
4. Previous Blood Disorders: Individuals with other myeloproliferative neoplasms, like polycythemia vera or essential thrombocythemia, may be at an increased risk of developing myelofibrosis.
5. Exposure to Radiation: Prolonged exposure to high levels of radiation, either through medical treatments or occupational exposure, has been linked to a higher risk of developing myelofibrosis.
6. Chemical Exposure: Some studies suggest a potential relationship between exposure to certain chemicals, like benzene, and an increased risk of myelofibrosis. However, more research is needed to establish a clear connection.
7. Family History: While it is not typically inherited, having a family history of myeloproliferative neoplasms or blood disorders may slightly increase the risk.
8. Inflammatory Conditions: Chronic inflammation, whether due to autoimmune disorders or other inflammatory conditions, may play a role in the development of myelofibrosis.
9. Viral Infections: In some cases, viral infections such as hepatitis or HIV have been suggested as potential triggers for myelofibrosis, though the association is not well-defined.
It’s essential to note that these risk factors do not guarantee the development of myelofibrosis, and the disease can occur in individuals without any known risk factors. If you have concerns about your risk or experience symptoms associated with myelofibrosis, it is better to contact a medical professional for proper evaluation & guidance.
Complications Of Myelofibrosis
Some common complications of myelofibrosis include:
1. Anemia: It often leads to a decrease in the growth of red blood cells, causing anemia. Anemia can result in fatigue, weakness, and shortness of breath.
2. Splenomegaly: The spleen is frequently enlarged in myelofibrosis as it tries to compensate for the lower production of blood cells in the bone marrow. A large spleen can cause discomfort or pain in the left upper abdomen.
3. Thrombocytopenia: It can reduce the production of platelets, increasing the risk of bleeding and bruising.
4. Leukocytosis: Some individuals having this rare disease may encounter an elevated white blood cell count, developing the risk of infections.
5. Blast Transformation: In rare cases, it may progress to acute leukemia, known as blast transformation. This transformation involves increased immature blood cells (blasts) in the bone marrow.
6. Bone Pain: Fibrous tissue replacing the normal bone marrow can cause bone pain and discomfort.
7. Fatigue: Anemia, coupled with the overall impact of the disease on the body, often leads to persistent fatigue.
8. Weight Loss: Some individuals with this medical condition may experience unintentional weight loss due to various factors, including decreased appetite and increased metabolic demands.
9. Portal Hypertension: Increased pressure in the portal vein (portal hypertension) can result from the enlargement of the spleen. This may lead to complications such as ascites (fluid accumulation in the abdomen) and varices (enlarged blood vessels in the esophagus or stomach, which can bleed).
10. Infections: The compromised immune system due to abnormalities in white blood cell production may increase susceptibility to infections.
11. Cardiac Complications: It can sometimes affect the heart, leading to heart-related complications.
How Is Myelofibrosis Diagnosed?
There is no single test that can confirm if you have this disease. Your doctor must do a physical exam, ask about your symptoms and medical history, and order blood and imaging tests. The most important test for diagnosing myelofibrosis is a bone marrow biopsy, which includes taking a small sample of your bone marrow from your hipbone and examining it under a microscope. The biopsy can show if there is scarring in your bone marrow and what types of blood cells are present.
Another test that can help with the diagnosis is a genetic test that finds mutations in certain genes involved in blood cell production. The most common gene mutation in myelofibrosis is called JAK2, which affects about half of the people with this disease. Other gene mutations include CALR and MPL, which are less common. Knowing which gene mutation you have can help your doctor determine your prognosis and treatment options.
Conclusion
In conclusion, myelofibrosis is a rare and chronic bone marrow disorder characterized by overproducing fibrous tissue, leading to compromised blood cell production. As research continues, a better understanding of myelofibrosis and advancements in treatment modalities offer hope for improved outcomes and enhanced patient care. Patients and their healthcare providers play a crucial role in navigating the complexities of this disease and tailoring treatment plans to individual needs.
Myelofibrosis treatment often involves a combination of medications, regular check-ups, and, in some cases, advanced therapies or even bone marrow transplants. These treatments come with exorbitant costs that can impair the financial stability of affected individuals and their families. A crowdfunding platform can bridge this financial gap by mobilizing the collective strength of a supportive community.












