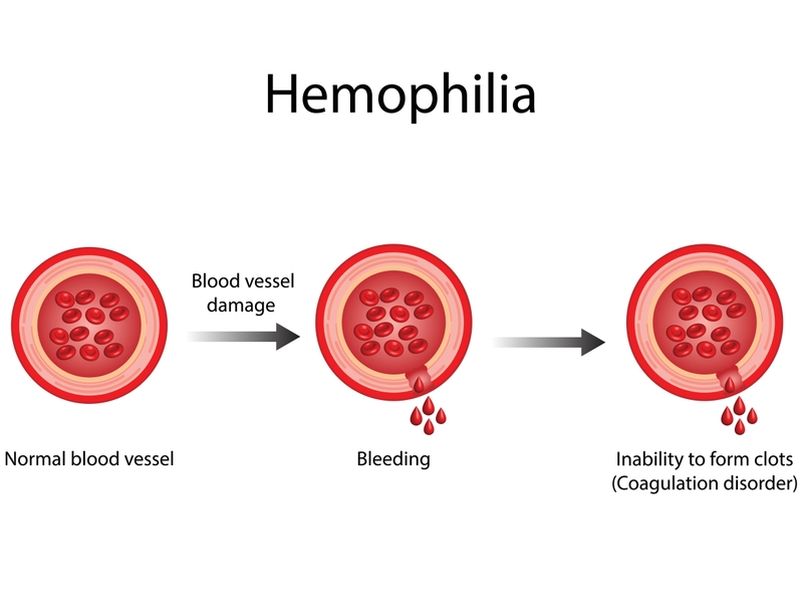
Haemophilia or hemophilia, a rare and potentially life-threatening genetic disorder, has long been a subject of both medical intrigue and concern. This inherited bleeding disorder is characterised by the deficiency or absence of clotting factors in the blood, impairing the body’s ability to form blood clots properly. As a result, individuals with haemophilia disease are prone to prolonged bleeding even after minor injuries, surgeries, or spontaneous internal bleeding episodes.
At the core of hemophilia lies a genetic anomaly, as it is typically inherited through the X chromosome. While both men and women can be carriers of the gene, it primarily affects males. Haemophilia A, the most common form of the ailment, results from a deficiency of clotting factor VIII, while a deficiency of factor IX causes Haemophilia B. The severity of the condition varies, classified as mild, moderate, or serious, depending on the degree of clotting factor deficiency.
The symptoms of haemophilia may manifest early in life, often becoming noticeable during infancy or childhood. Common signs include prolonged bleeding from cuts or injuries, spontaneous joint bleeds, and easy bruising. Individuals with severe haemophilia may experience spontaneous bleeding without an apparent cause, particularly into joints and muscles, leading to chronic pain and, if left untreated, potential joint damage.
Diagnosing haemophilia involves a comprehensive evaluation of medical history, family history, and specific blood tests to determine clotting factor levels. Due to its rarity and varied presentations, diagnosis can be challenging, requiring the expertise of haematologists and specialised laboratories equipped to assess clotting factor deficiencies accurately.
While haemophilia has no cure, advancements in medical science have paved the way for effective management and treatment strategies. The main goal of haemophilia treatment is to replace the deficient clotting factors, either through regular prophylactic infusions or on-demand therapy in response to bleeding events. Recombinant clotting factor concentrates, derived from human or animal plasma, have significantly improved the quality of life for individuals with hemophilia.
In India, the economic aspects of haemophilia treatment play a pivotal role in shaping the accessibility and affordability of care. The cost of clotting factor concentrates, diagnostic tests, and other related medical expenses can pose significant financial burdens for patients and their families.
As we delve into the intricate facets of hemophilia – from its genetic underpinnings to the challenges in diagnosis, available treatment options, and the treatment costs in India – it becomes evident that a comprehensive understanding of this disorder is essential for fostering awareness, encouraging early diagnosis, and facilitating improved healthcare outcomes for individuals grappling with haemophilia.
Table of Contents
Haemophilia Symptoms
The symptoms of haemophilia can vary in severity based on the level of clotting factor in the blood. Here are some common symptoms:
1. Excessive Bleeding: Individuals with haemophilia may bleed for a more extended period than usual after an injury, surgery, or dental work. They may also experience spontaneous bleeding, which can occur internally in joints & muscles or externally from minor cuts or injuries.
2. Bruising: Easy bruising is common in people with haemophilia. Bruises may occur from minimal trauma or without an apparent cause.
3. Joint Pain and Swelling: Internal bleeding into joints is a hallmark symptom of haemophilia. This often affects weight-bearing joints such as the knees, ankles, and elbows. If not treated promptly, the bleeding into joints can lead to pain, swelling, and long-term damage and deformities.
4. Muscle Pain: Bleeding into muscles can cause pain and swelling. This may result in a tight or tense feeling in the affected muscle.
5. Nosebleeds: Frequent or prolonged nosebleeds may occur in individuals with haemophilia.
6. Blood in Urine or Stool: Internal bleeding can sometimes lead to blood in the stool or urine. This can be a more severe symptom and requires immediate medical attention.
7. Excessive Bleeding in Women: Women with haemophilia may experience heavier than usual menstrual bleeding or bleeding after childbirth.
It’s essential to note that the severity of symptoms can vary among individuals with haemophilia. Some may have mild symptoms and only experience bleeding in response to significant trauma or surgery, while others may have severe symptoms with spontaneous bleeding into joints and muscles.
Early diagnosis and proper management of haemophilia are vital to prevent complications and improve the quality of life for individuals with this condition. Treatment often involves the replacement of the deficient clotting factor through intravenous infusions. People with haemophilia should work closely with medical professionals to develop a personalised treatment plan tailored to their specific needs and circumstances.
Haemophilia Treatments
Depending on the type, severity, and frequency of bleeding episodes, Haemophilia can be treated with various methods. Some of the common treatments include:
– Factor replacement therapy: This is the primary treatment for haemophilia, which involves injecting the missing clotting factor into the bloodstream through a vein. This can be done on demand when a bleeding episode occurs or as a preventive measure to reduce the risk of bleeding.
– Gene therapy: This emerging treatment option aims to correct the faulty gene responsible for haemophilia. This can be done using a virus or other vector to deliver a regular gene copy into the cells that produce clotting factors. This can potentially cure haemophilia or reduce the need for factor replacement therapy.
– Regular monitoring: People with haemophilia need regular check-ups with their doctors to monitor their clotting factor levels and overall health. They also need to keep track of their bleeding episodes and report any changes or complications.
– Physical therapy: This can help manage joint pain and improve mobility in people with haemophilia who have joint damage due to repeated bleeding. Physical therapy can include exercises, massage, heat, ice, or other modalities to reduce inflammation and improve function.
– Medications: Certain medications may be prescribed to control bleeding or prevent complications in people with haemophilia. For example, antifibrinolytic drugs such as tranexamic acid or aminocaproic acid can help prevent blood clots from breaking down too quickly. Desmopressin (DDAVP) can stimulate the release of factor VIII in some people with mild haemophilia A. Antibiotics can prevent infections from contaminated blood products or wounds.
Haemophilia is a lifelong condition that requires careful management and support. However, with proper treatment and care, people with haemophilia can lead normal and productive lives.
What Is Haemophilia?
Hemophilia is a rare genetic disorder that impairs the body’s ability to limit blood clotting or coagulation, which is the process that helps stop bleeding. People with haemophilia experience prolonged bleeding, both internal and external, after an injury or surgery.
The disorder is typically inherited, meaning it is passed down from parents to their children through a defective gene on the X chromosome. There are several types of haemophilia, the two most common being haemophilia A and haemophilia B. The difference between them lies in the specific clotting factor that is deficient.
A deficiency of clotting factor VIII causes Hemophilia A, while haemophilia B is caused by a deficiency of clotting factor IX. These clotting factors are proteins essential for the normal blood clotting process. The severity of haemophilia can vary, with individuals classified as having mild, moderate, or severe forms of the disorder based on the amount of clotting factor in their blood.
Treatment typically involves replacing the deficient clotting factor through intravenous infusion of clotting factor concentrates. With proper treatment and management, individuals with haemophilia can lead relatively normal and healthy lives. However, ongoing medical supervision and careful attention to bleeding episodes are crucial for optimal outcomes.
Haemophilia Causes
Haemophilia is a rare disorder that impairs the body’s ability to control blood clotting, leading to prolonged bleeding episodes. There are two primary kinds of haemophilia: Haemophilia A, resulting from a deficiency of clotting factor VIII, & Haemophilia B, caused by a deficiency of clotting factor IX. The causes of haemophilia are primarily genetic, and the disorder is usually inherited in an X-linked recessive pattern.
Here’s a more detailed explanation:
1. Genetic Inheritance:
– Haemophilia is caused by gene mutations that provide instructions for making clotting factors VIII or IX, located on the X chromosome. The X-linked recessive pattern means the genes responsible for haemophilia are on the X chromosome. The disorder predominantly affects males since females have two X chromosomes (XX) and males have one X and Y chromosome (XY).
– If a female carries a mutated gene on one of her X chromosomes, she is considered a carrier and usually does not show symptoms. However, if she has a son, there is a 50% probability that he will inherit the mutated gene and develop haemophilia. If she has a daughter, there is a 50% likelihood that the daughter will be a carrier like her.
2. Spontaneous Mutation:
– In some cases, individuals may develop haemophilia due to spontaneous mutations in the clotting factor genes. This can occur without any family history of the disorder. Such cases are relatively rare.
3. Family History:
– Individuals with a family history of haemophilia are at an increased risk of inheriting the disorder. If a person has a close relative, such as a father, brother, or maternal uncle, with haemophilia, there is a higher likelihood of being at risk.
4. Carrier Status:
– Carrier females, while not having the disorder themselves, can transfer the mutated gene to their children. If a carrier female has a son, there is a 50% probability that he will inherit the mutated gene & develop haemophilia. Carrier females may also have mild bleeding tendencies, depending on the level of clotting factor produced by the non-mutated X chromosome.
It’s important to note that while haemophilia is primarily a genetic disorder, the severity of symptoms can vary. Advances in medical treatment, including the availability of clotting factor concentrates, have significantly improved the quality of life for individuals with haemophilia. Genetic counselling is often preferred for individuals with a family history of the disorder to understand the risks and make informed decisions.
Haemophilia Types
Hemophilia or Hemophiliais a rare genetic disorder affecting the blood’s clot ability. It is characterised by a deficiency or absence of certain clotting factors, proteins essential for blood clotting. There are several types of haemophilia, the most common being Hemophilia A and Hemophilia B. Here’s a detailed explanation of each:
1. Hemophilia A:
– Cause: Hemophilia A is caused by a deficiency or absence of clotting factor VIII (FVIII), which is necessary for the formation of blood clots.
– Inheritance: It is inherited in an X-linked recessive manner, meaning the defective gene is on the X chromosome. Since men have only X chromosome, they are more commonly affected than females. However, females can be carriers of the gene and may show mild symptoms.
2. Hemophilia B (Christmas Disease):
– Cause: Hemophilia B is caused by a deficiency or absence of clotting factor IX (FIX). It is also known as Christmas Disease, named after the first patient diagnosed with this type of hemophilia.
– Inheritance: Like Hemophilia A, Hemophilia B is inherited in an X-linked recessive manner. It primarily affects males, and females can be carriers.
3. Hemophilia C:
– Cause: Hemophilia C is much less common than Hemophilia A and B. It is generally caused by a deficiency of clotting factor XI (FXI).
– Inheritance: Unlike Hemophilia A and B, Hemophilia C follows an autosomal recessive pattern of inheritance. Both males & females are equally affected, and carriers may not show symptoms.
4. Acquired Hemophilia:
– Cause: Acquired haemophilia is a rare disorder that is not inherited but develops later in life. It develops when the immune system mistakenly affects clotting factors.
– Occurrence: Unlike the inherited forms, acquired hemophilia can affect both males & females at any age.
Haemophilia Treatment Cost In India
The cost of replacement therapy varies depending on the type and severity of haemophilia, the frequency and duration of treatment, and the availability and quality of clotting factors. In India, the cost of replacement therapy ranges from Rs. 1,95,000 to Rs. 5,52,500 per year, according to the severity of the disorder in the patient. However, this cost may not include other expenses such as hospitalisation, surgery, physiotherapy, or laboratory tests.
One of the challenges faced by people with haemophilia in India is the limited availability and accessibility of clotting factors. According to a report by The Times of India, only 15% of people with hemophilia in India receive adequate treatment. The rest either depend on blood transfusions, which carry the risk of infections and antibodies, or suffer from chronic pain and disability.
Haemophilia is a lifelong condition that requires regular monitoring and treatment. However, with proper care and support, people with haemophilia can lead healthy and everyday lives. If you or your loved one has haemophilia, you can consult a haematologist or a haemophilia treatment centre to find the best treatment options for your condition.
Risk Factors & Complications Of Haemophilia
Haemophilia is a rare genetic disorder characterised by the deficiency or absence of specific blood clotting factors, usually Factor VIII (hemophilia A) or Factor IX (hemophilia B). These clotting factors are essential for proper blood clotting, and their deficiency can lead to prolonged bleeding and difficulty in clot formation. Here, I’ll discuss the risk factors and complications associated with haemophilia.
Risk Factors:
1. Genetic Inheritance:
– Haemophilia is an inherited disorder primarily passed down through the X chromosome.
– The most common form is X-linked recessive, meaning it primarily affects males. Females can be carriers, but they typically do not experience symptoms.
2. Family History:
– Individuals with a family history of haemophilia are at a higher risk. If a close family member, such as a father or brother, has the condition, the likelihood of inheriting it increases.
3. Gender:
– While both males & females can carry the gene for hemophilia, it predominantly affects males. Females with one affected X chromosome are typically carriers but may not show symptoms.
4. Spontaneous Mutation:
– In some cases, individuals with no family history of haemophilia may still develop the condition due to spontaneous mutations in the genes responsible for blood clotting factors.
Complications:
1. Bleeding Episodes:
– The primary complication of haemophilia is spontaneous and prolonged bleeding, often from minor injuries or even without an apparent cause.
– Bleeding can occur internally in joints, muscles, or organs, leading to pain, swelling, and potential long-term damage.
2. Joint Damage:
– Recurrent bleeding into joints, especially weight-bearing joints like knees and ankles, can cause chronic joint damage. This can result in limited mobility, deformities, and chronic pain.
3. Intracranial Hemorrhage:
– Severe cases of hemophilia may lead to spontaneous bleeding in the brain (intracranial haemorrhage), which can result in neurological damage and be life-threatening.
4. Soft Tissue Hematomas:
– Bleeding into soft tissues can lead to the formation of hematomas, causing pain, swelling, and potential complications if not adequately managed.
5. Muscle Hemorrhages:
– Bleeding into muscles can cause compartment syndrome, a condition where increased pressure within the muscle compartments impairs blood flow and can lead to tissue damage.
6. Infections and Complications from Treatment:
– Regular treatment with clotting factor concentrates or other medications can increase the risk of developing inhibitors (antibodies) against these clotting factors, making treatment more challenging.
– The use of blood products also carries a risk of infection, such as hepatitis or HIV, although modern treatments have significantly reduced this risk.
7. Psychosocial Impact:
– Living with a chronic condition like haemophilia can have psychological and social implications, leading to anxiety, depression, and challenges in daily life.
Effective management of haemophilia involves a combination of preventive measures, prompt treatment of bleeding episodes, and ongoing medical care to minimise complications. Advances in treatment options, including gene therapy, have improved the outlook for individuals with haemophilia, but comprehensive care and support remain crucial for a better quality of life.
Diagnosis Of Haemophilia
Diagnosing haemophilia involves a combination of clinical evaluation, medical history assessment, and laboratory tests. Here are the key steps in diagnosing haemophilia:
1. Clinical Evaluation:
– Medical History: A thorough study of the patient’s medical history is essential. The doctor will inquire about any family history of bleeding disorders, as haemophilia is often inherited.
– Symptoms: The doctor will assess symptoms such as easy bruising, prolonged bleeding after injuries or surgeries, and spontaneous bleeding.
– Family History: Hemophilia is often a genetic disorder, so a family history of the condition is significant.
2. Physical Examination:
– The physician will conduct a physical evaluation to look for signs of bleeding, such as bruising, joint swelling, and any other abnormal bleeding.
3. Laboratory Tests:
– Complete Blood Count (CBC): A CBC can reveal the number of platelets and red and white blood cells in the blood.
– Clotting Factor Tests: Specific blood tests, such as partial thromboplastin time (PTT) and activated partial thromboplastin time (aPTT), can help identify abnormalities in clotting factors. In haemophilia, there is typically a prolonged PTT.
– Factor Assays: To determine the specific type of haemophilia (A or B), factor assays can be conducted to measure the levels of clotting factors VIII and IX.
4. Genetic Testing:
– Genetic testing may be preferred to confirm the diagnosis and identify the specific genetic mutation responsible for haemophilia. This is particularly useful for family planning and understanding the inheritance pattern.
5. Joint Imaging:
– In severe cases of haemophilia, joint damage can occur due to bleeding into the joints. X-rays or other imaging studies may be done to assess the extent of joint damage.
6. Specialized Tests:
– In some cases, other specialised tests may be performed to assess overall clotting function and rule out other bleeding disorders.
It’s important to note that a comprehensive evaluation by a healthcare professional, often a haematologist, is crucial for an accurate diagnosis. If there is a suspicion of haemophilia based on the initial assessment, further testing will be conducted to confirm the diagnosis & determine the severity of the condition. Early diagnosis is vital for the management and prevention of complications associated with hemophilia.
Conclusion
In conclusion, understanding haemophilia is crucial for both patients and the broader community to foster a supportive environment and ensure optimal management of the condition. Haemophilia, characterised by impaired blood clotting, presents with distinctive symptoms that range from mild to severe, impacting the quality of life for those affected. While genetic factors play a central role in the development of haemophilia, advancements in medical science have shed light on potential treatment options and preventive measures.
In the Indian context, where healthcare accessibility and affordability are critical considerations, awareness about haemophilia is pivotal. Recognising the signs, seeking prompt medical consultation, and adhering to treatment plans can empower individuals with hemophilia to lead fulfilling lives. However, it is imperative to acknowledge the economic aspects of managing haemophilia, including the costs associated with treatments, medications, and supportive care.
In essence, the comprehensive understanding of haemophilia, encompassing its symptoms, causes, and treatment options, is instrumental in fostering a compassionate and informed approach towards those affected by this condition.
Haemophilia treatment requires a lifelong commitment to regular and expensive medications, frequent hospital visits, and sometimes specialised care. Many individuals and families in India face financial constraints that make it challenging to afford these essential treatments. A crowdfunding platform provides a collective solution, allowing the community to come together to financially support those in need.












