Graves’ Disease, an autoimmune disorder that primarily affects the thyroid gland, is a complex and often misunderstood condition. Named after the Irish physician Robert J. Graves, who first described it in the early 19th century, this disorder is characterised by an overactive thyroid, leading to a variety of symptoms and potential complications. In this complete guide, we will try to understand the intricate aspects of Graves’ Disease, exploring its symptoms, treatments, and underlying causes.
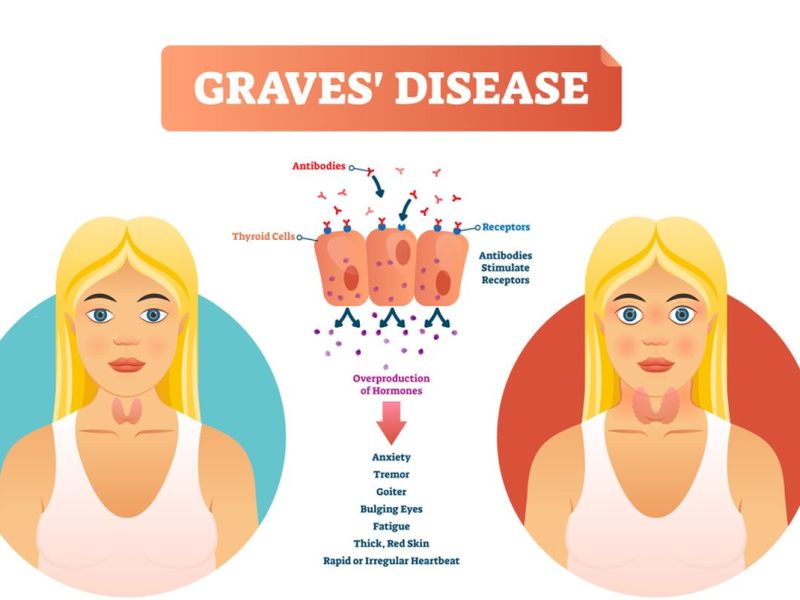
Understanding Graves’ Disease requires a grasp of the thyroid’s role in the body. The thyroid gland, located in the neck, develops hormones crucial for regulating metabolism. In Graves’ Disease, the immune system mistakenly affects the thyroid, causing it to have excessive amounts of thyroid hormones. This hormonal imbalance triggers a range of symptoms that can significantly impact an individual’s well-being.
One of the primary symptoms of Graves’ Disease is hyperthyroidism, characterised by rapid heartbeat, weight loss, and increased sensitivity to heat. Patients may also experience anxiety, irritability, and insomnia. The eyes can be affected as well, leading to a condition known as Graves’ ophthalmopathy, which manifests with bulging eyes, double vision, and eye irritation. The complexity of symptoms makes diagnosis challenging, often requiring a combination of clinical evaluation, blood tests, and imaging studies.
Treatment strategies for Graves’ Disease aim to restore hormonal balance and manage symptoms effectively. Antithyroid medications, like methimazole or propylthiouracil, are commonly prescribed to inhibit the overproduction of thyroid hormones. Radioactive iodine therapy, another option, involves the use of a radioactive substance to shrink the thyroid and reduce hormone production. In serious cases, surgical intervention to remove the thyroid gland may be considered. Each treatment approach comes with its set of considerations & potential side effects, highlighting the importance of personalised medical management.
The precise causes of Graves’ Disease remain elusive, but genetic & environmental factors are believed to play significant roles. Family history and certain genes may increase susceptibility to the disorder, while stress and infections have been identified as potential triggers. The interplay of these factors in the context of an individual’s immune system contributes to the development of Graves’ Disease, emphasising the need for ongoing research to unravel the complexities of its origin.
As we embark on this exploration of Graves’ Disease, it is essential to recognise the impact it can have on individuals’ lives. By shedding light on its symptoms, treatments, and potential causes, we aim to empower readers with knowledge and foster a greater understanding of this autoimmune condition. Stay tuned for in-depth insights into each facet of Graves’ Disease, providing a comprehensive resource for those affected and those seeking to expand their awareness of this intricate medical condition.
Table of Contents
Graves’ Disease Symptoms
Graves’ disease is an autoimmune ailment that causes overactivity of the thyroid gland (hyperthyroidism). It is the most common cause of hyperthyroidism. The symptoms of Graves’ disease can vary in severity and may include:
1. Enlarged Thyroid (Goiter): Graves’ disease often causes the thyroid gland to become enlarged, causing a noticeable swelling in the neck.
2. Hyperthyroidism Symptoms:
– Weight loss: Despite increased appetite, individuals may experience weight loss.
– Increased heart rate (tachycardia): The heart may beat faster than normal.
– Irregular heartbeat (arrhythmia): Abnormal heart rhythms can occur.
– Nervousness and irritability: Patients may feel anxious and irritable.
– Tremors: Fine trembling or shaking of the hands or fingers.
– Sweating: Excessive sweating, even in cooler temperatures.
– Fatigue: Despite increased activity, individuals may feel tired and weak.
3. Eye Changes (Graves’ Ophthalmopathy):
– Bulging eyes (exophthalmos): The eyes may appear to protrude or bulge.
– Red or swollen eyes: Irritation and inflammation of the eyes can occur.
– Double vision: Some individuals may experience double vision.
4. Skin Changes:
– Warm and moist skin: The skin may feel warm and sweaty.
– Thin and brittle hair: Hair may become fine and break more easily.
5. Menstrual Irregularities: Women with Graves’ disease may experience irregular menstrual cycles.
6. Muscle Weakness: Some individuals may experience muscle deficiency, generally in the thighs & upper arms.
It’s vital to remember that not everyone with Graves’ disease will face all of these symptoms, & the severity can differ from person to person. If you suspect you have Graves’ disease or are experiencing symptoms of hyperthyroidism, it is crucial to seek medical attention for appropriate diagnosis & management.
Graves’ Disease Treatments
There are three main types of treatments for Graves’ disease: anti-thyroid drugs, radioactive iodine therapy and surgery. Each of these treatments has its own advantages & disadvantages, & the choice depends on various factors, like the severity of the disease, the patient’s age, preference, medical history and availability of resources. In this article, we will discuss each of these treatments in detail and their cost in India.
Anti-thyroid drugs
Anti-thyroid drugs are medications that block the production of thyroid hormone by the thyroid gland. They are usually the first line of treatment for Graves’ disease, especially for mild to moderate cases, pregnant women and children. The most commonly used anti-thyroid drugs are methimazole and propylthiouracil (PTU). These drugs are taken orally, usually once or twice a day, for 12 to 18 months or longer. The dose is adjusted as per the patient’s response & thyroid function tests.
Anti-thyroid drugs can effectively control the symptoms of hyperthyroidism, but they do not cure the underlying cause of this disease. Therefore, there is a high chance of relapse after stopping the medication. Some patients may need to take anti-thyroid drugs for life or switch to another treatment option if they do not achieve remission. Anti-thyroid drugs can also cause side effects, like rash, itching, joint pain, fever, liver damage and a rare but serious condition called agranulocytosis, which is a low white blood cell count that increases the risk of infection.
The cost of anti-thyroid drugs in India varies depending on the brand, dosage and duration of treatment. The average price of methimazole is around Rs. 50 to Rs. 100 per month, while the average cost of PTU is around Rs. 200 to Rs. 400 per month.
Radioactive iodine therapy
It is a treatment that involves taking a capsule or liquid containing a small quantity of radioactive iodine (I-131). The thyroid gland absorbs the radioactive iodine and destroys the overactive thyroid cells, reducing the production of thyroid hormone. Radioactive iodine therapy is usually a one-time treatment that can effectively cure Graves’ disease in most cases. It is suitable for patients who have severe or recurrent hyperthyroidism, who cannot tolerate or are allergic to anti-thyroid drugs, or who do not want surgery.
Radioactive iodine therapy has some advantages over other treatments, such as being simple, safe and cost-effective. It does not require hospitalisation or anaesthesia and has few side effects. However, it also has some disadvantages, such as being irreversible and causing hypothyroidism (underactive thyroid) in up to 80% of patients within a year after treatment. Hypothyroidism is a medical state where the thyroid gland does not develop enough thyroid hormone, causing symptoms such as fatigue, weight gain, depression & cold intolerance. Patients who develop hypothyroidism after radioactive iodine therapy are required to consume thyroid hormone replacement pills for life.
The cost of radioactive iodine therapy in India depends on the dose of radioactive iodine required and the hospital charges. The average cost of radioactive iodine therapy in India ranges from Rs. 15,000 to Rs. 25,000.
Surgery
Surgery is a treatment that involves removing all or part of the thyroid gland (thyroidectomy). Surgery is usually reserved for patients who have very large goitres (enlarged thyroid glands) that cause compression symptoms such as difficulty breathing or swallowing, who have eye problems due to Graves’ disease (Graves’ ophthalmopathy), who have suspicious nodules or cancer in the thyroid gland, or who are not suitable for or refuse anti-thyroid drugs or radioactive iodine therapy.
Surgery can cure Graves’ disease by removing the source of excess thyroid hormone production. However, surgery also has some risks and complications, such as bleeding, infection, damage to the nearby nerves that control the voice box (laryngeal nerves) or the parathyroid glands that regulate calcium levels (hypoparathyroidism), and hypothyroidism. Patients who undergo surgery need to take thyroid hormone replacement pills for life and may also need to take calcium & vitamin D supplements.
The cost of surgery in India depends on the kind of surgery, the surgeon’s fees, the hospital charges and the post-operative care. The average cost of surgery in India ranges from Rs. 50,000 to Rs. 1,50,000.
What Is Graves Disease?
Graves’ disease is an autoimmune disorder that harms the thyroid gland, a small butterfly-shaped gland positioned in the neck, just beneath the Adam’s apple. This condition leads to overactivity of the thyroid gland, a condition known as hyperthyroidism.
In Graves’ disease, the immune system mistakenly creates antibodies that stimulate the thyroid gland to develop an excessive quantity of thyroid hormones, primarily thyroxine (T4) & triiodothyronine (T3). These hormones are vital in regulating the body’s metabolism, affecting various processes such as heart rate, energy levels, and temperature.
Thyroid hormone affects several body parts and bodily functions, such as:
– Heart rate and blood pressure
– Body temperature
– Muscle strength and coordination
– Mood and mental function
– Growth and development
– Reproduction and menstrual cycle
– Appetite and weight
Graves Disease Causes
The exact cause of Graves’ disease is not fully known, but it is believed to involve a mixture of genetic, environmental, & immunological factors. Here are some factors that may contribute to the development of Graves’ disease:
1. Genetic Predisposition: There is a strong genetic component associated with this disease. Individuals with a family history of autoimmune disorders, including Graves’ disease, have a higher risk of developing the condition.
2. Autoimmune Response: Graves’ disease is classified as an autoimmune disorder, which means the immune system mistakenly attacks its tissues. In this medical case, the immune system produces antibodies known as thyroid-stimulating immunoglobulins (TSI) that mimic the action of thyroid-stimulating hormone (TSH). These antibodies stimulate the thyroid gland to develop excess thyroid hormones.
3. Environmental Triggers: Certain environmental factors may trigger or exacerbate the development of Graves’ disease in genetically predisposed individuals. Factors such as stress, infections, and smoking have been suggested as possible triggers.
4. Hormonal Factors: This disease is more common in women than in men, and it often occurs during or after pregnancy. Changes in hormonal levels, especially during pregnancy or menopause, may influence the development of the disease.
5. Infections: Some infections, particularly viral and bacterial infections, may play a role in triggering autoimmune responses. In some cases, infections may act as a catalyst for the development of Graves’ disease in susceptible individuals.
6. Stress: Stress is believed to have an impact on the immune system and may contribute to the onset or exacerbation of autoimmune disorders. While stress alone is not a direct cause, it can be a contributing factor.
It’s important to note that the interplay of these factors is complex, and the exact mechanisms leading to Graves’ disease may vary among individuals. Additionally, only some people with a genetic predisposition or exposure to potential triggers will develop the condition.
Graves Disease Diagnosis
To diagnose Graves’ disease, your doctor will ask you about your medical history, family history, and symptoms. They will also do a physical examination to check your blood pressure, heart rate, thyroid size, and eye appearance. In addition, they may order some tests to confirm the diagnosis, such as:
– Blood tests: These tests observe the levels of thyroid hormones (T3 & T4) & thyroid-stimulating hormone (TSH) in your blood. People with this disease usually have high levels of T3 & T4 and low levels of TSH. They may also have antibodies against the thyroid receptor (TRAb), which is responsible for stimulating the thyroid gland to produce more hormones.
– Radioactive iodine uptake test: This test involves swallowing a small amount of radioactive iodine and then measuring how much of it is absorbed by your thyroid gland. A high uptake of iodine indicates that your thyroid is overactive & producing too much hormone. This test may also show a characteristic pattern of iodine distribution in your thyroid gland that is typical of Graves’ disease.
– Ultrasound: This medical test utilises sound waves to develop a picture of your thyroid gland. It can show if your thyroid is enlarged or has any nodules or cysts.
– Imaging tests: If the detection of Graves’ disease is not clear from the above tests, your doctor may order special imaging tests, like a CT scan or MRI, to look for other causes of hyperthyroidism or to evaluate the extent of eye involvement.
Prognosis (Outlook) For Graves’ Disease
People with Graves’ disease may be able to manage their condition with medication & other treatments. A small percentage of people with Graves’ disease, especially those with mild Graves’ disease, may go into remission and no longer need treatment. The remission may only be temporary, particularly among children.
However, some people may need lifelong treatment to keep their thyroid hormone levels in balance and prevent complications such as cardiovascular disease or osteoporosis. Regular follow-up visits with your medical provider are vital to monitor your condition and adjust your treatment as needed.
Living with Graves’ disease can be challenging, but there are some steps you can take to cope better and improve your quality of life, such as:
– Eating a balanced diet that involves enough calories, protein, calcium and vitamin D to support your metabolism, muscles, bones and overall health.
– Avoiding foods or supplements that contain excess iodine, such as seaweed, kelp, iodised salt or multivitamins with iodine.
– Avoiding caffeine, alcohol, tobacco and other stimulants that can worsen your symptoms or interfere with your medication.
Risk Factors For Graves’ Disease
While the exact reason for Graves’ disease is not well understood, several risk factors may contribute to its development. It’s important to note that having one or more risk factors doesn’t guarantee the development of Graves’ disease, and the interplay of genetic and environmental factors is complex. Here are some recognised risk factors:
1. Genetics: Individuals with a family history of autoimmune disorders, including Graves’ disease, are at a higher risk. There seems to be a genetic predisposition, and specific genes associated with the immune system may contribute to the development of autoimmune diseases.
2. Gender: Graves’ disease is more common in women than in men. The female-to-male ratio is estimated to be about 5:1. The reason for this gender difference is not fully known, but hormonal factors may play a key role.
3. Age: While this disease can develop at any age, it most commonly begins between the ages of 30 and 50. It is less common in children and older adults.
4. Stress: There is some evidence that stress may trigger or exacerbate autoimmune conditions, including Graves’ disease. However, the relationship between stress and the development of Graves’ disease is complex and not fully understood.
5. Pregnancy and childbirth: Women who have recently given birth may be at an increased risk of developing Graves’ disease. Additionally, pregnant women with a history of Graves’ disease may experience a worsening of symptoms during pregnancy.
6. Smoking: Cigarette smoking has been identified as a potential environmental risk factor for Graves’ disease. Smokers, especially women, are at a higher risk compared to non-smokers.
7. Infections: Some infections, particularly viral & bacterial infections, have been suggested as potential triggers for Graves’ disease. However, the relationship between specific infections and the development of the condition needs to be well-established.
It’s important to note that while these factors are associated with a higher risk of Graves’ disease, many people with the condition do not have any identifiable risk factors. Additionally, more research is required to fully understand the complex interplay of genetic & environmental factors in the development of autoimmune disorders like Graves’ disease. If you suspect you have Graves’ disease or are at risk, it’s crucial to contact a healthcare professional for proper diagnosis and management.
Complications Of Graves’ Disease
Graves’ disease is an autoimmune disorder that generally influences the thyroid gland, leading to the overproduction of thyroid hormones (hyperthyroidism). This condition can result in various complications affecting different organs and systems in the body. Some of the complications associated with Graves’ disease include:
1. Thyroid-Related Complications:
– Thyrotoxicosis: Excess production of thyroid hormones can lead to thyrotoxicosis, causing symptoms such as weight loss, rapid heartbeat, sweating, and anxiety.
– Goiter: An enlarged thyroid gland may develop, causing a visible swelling in the neck.
2. Eye Complications (Graves’ Ophthalmopathy or Thyroid Eye Disease):
– Proptosis (Exophthalmos): Bulging of the eyes is a characteristic feature, leading to irritation, dryness, and sometimes double vision.
– Eye discomfort: Pain, redness, and sensitivity to light are common symptoms.
– Optic nerve compression: In severe cases, pressure on the optic nerve can cause vision impairment.
3. Skin Complications:
– Dermatopathy: Some individuals with Graves’ disease may develop a condition known as pretibial myxedema, which causes thickening & reddening of the skin on the shins.
4. Cardiovascular Complications:
– Increased heart rate: Hyperthyroidism can lead to an elevated heart rate, palpitations, and increased risk of arrhythmias.
– Hypertension: Elevated blood pressure may occur, increasing the risk of cardiovascular problems.
5. Musculoskeletal Complications:
– Osteoporosis: Long-term hyperthyroidism can lead to bone loss, increasing the risk of fractures.
– Muscle weakness: Some individuals may experience muscle weakness and fatigue.
6. Reproductive Complications:
– Menstrual irregularities: Women with this disease may experience changes in their menstrual cycles.
– Fertility issues: Both men and women may face fertility problems.
7. Psychological Complications:
– Anxiety and irritability: Hyperthyroidism can contribute to psychological symptoms.
– Emotional disturbances: Depression or mood swings may occur.
8. Thyroid Storm:
– Rare but severe complication: It is a life-threatening condition characterised by extremely high levels of thyroid hormones, leading to symptoms such as fever, rapid heart rate, and altered mental status.
It’s important to note that not everyone with Graves’ disease will experience all these complications, and the severity of complications can vary among individuals.
Conclusion
In conclusion, the blog on Graves’ Disease provides a comprehensive overview of this autoimmune disorder, highlighting its symptoms, treatments, and causes. By delving into the intricate interplay of the immune system and thyroid function, the blog equips readers with valuable insights into recognising and managing Graves’ Disease. From exploring conventional medical interventions to considering lifestyle adjustments, the piece offers a holistic perspective on coping with this condition. Overall, this complete article is a valuable resource for those seeking a deeper understanding of Graves’ Disease & empowers patients and their families to make a well-informed decision regarding their health.
Graves’ Disease treatment often involves medications, surgeries, and regular medical consultations. These expenses can quickly accumulate, placing a heavy financial burden on individuals and their families.Crowdfunding platforms provide a collective opportunity for friends, family, and even strangers to contribute, making a significant impact on the overall financial burden.












