Cervical spondylosis, a prevalent and often misunderstood condition, encompasses a range of degenerative changes that affect the cervical spine, primarily occurring with age. This degeneration can lead to various symptoms, ranging from mild discomfort to severe pain and neurological complications. Understanding the intricacies of cervical spondylosis is crucial for effective management and prevention.
The symptoms of cervical spondylosis can manifest in diverse ways, impacting an individual’s daily life. Neck pain, a hallmark symptom, often radiates to the shoulders and arms, accompanied by stiffness and reduced range of motion. Headaches, particularly at the back of the head, are common, reflecting the intricate relationship between the cervical spine and the nervous system. Additionally, individuals may experience numbness, tingling, or weakness in the arms and hands, signaling potential nerve compression.
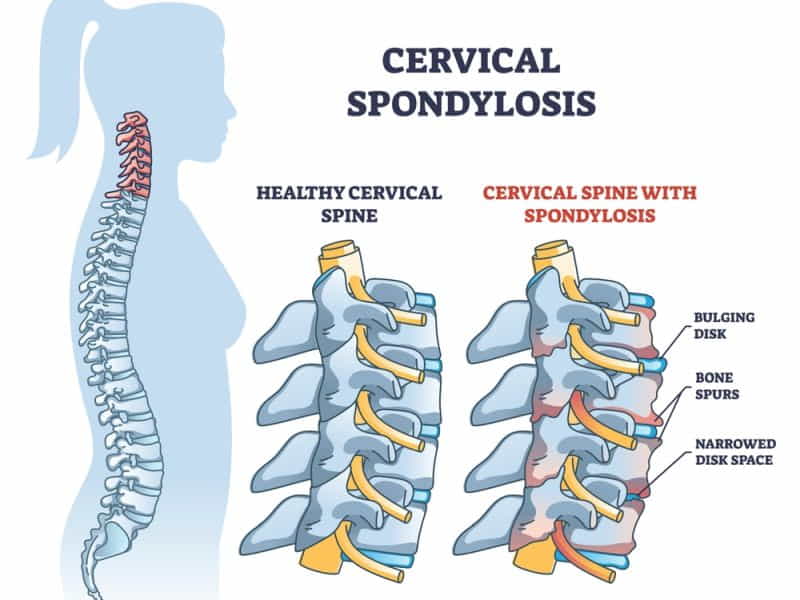
The root causes of cervical spondylosis are multifaceted, with age being a predominant factor. As the spine undergoes wear and tear over time, intervertebral discs lose their elasticity and water content, contributing to the development of osteophytes or bone spurs. These bony outgrowths can impinge on surrounding nerves, resulting in pain and discomfort. Other factors such as genetic predisposition, prolonged poor posture, and repetitive stress on the neck also play pivotal roles in the development of cervical spondylosis.
Management of cervical spondylosis involves a multidimensional approach, combining conservative measures and, in severe cases, surgical intervention. Non-surgical treatments encompass lifestyle modifications, physical therapy, and medications to alleviate pain and inflammation. Targeted exercises and stretches help improve neck strength and flexibility. In cases where conservative methods prove inadequate, surgical options, such as discectomy or spinal fusion, may be considered to release pressure on affected nerves and restore stability to the spine.
In navigating cervical spondylosis, awareness and early intervention are pivotal. A comprehensive understanding of the symptoms, causes, & available treatments empowers individuals and healthcare professionals alike to address this degenerative condition effectively. By prioritizing preventive measures and adopting a holistic approach to care, the impact of cervical spondylosis on quality of life can be minimized, allowing individuals to maintain optimal neck health throughout their lives.
Table of Contents
Cervical Spondylosis Symptoms
The symptoms of cervical spondylosis can differ from person to person, and some individuals may not experience any noticeable symptoms. However, common symptoms may include:
1. Neck pain: Persistent or intermittent pain in the neck is a common symptom. The pain may be localized to the shoulders & arms.
2. Stiffness: Reduced range of motion and stiffness in the neck, making it difficult to turn the head or tilt it in different directions.
3. Headaches: Cervical spondylosis can cause headaches, especially at the base of the skull. These headaches may be associated with muscle tension or nerve irritation.
4. Numbness and tingling: Compression of nerves in the cervical spine can lead to sensations of numbness, tingling, or deficiency in the arms, hands, & fingers.
5. Muscle weakness: As the condition progresses, muscle weakness may occur, affecting the arms and hands. This can impact fine motor skills and grip strength.
6. Loss of coordination: In severe cases, cervical spondylosis may affect the coordination of movements, leading to balance problems and difficulty walking.
7. Radiating pain: Pain that starts from the neck down to the shoulders, arms, and even the hands. This is often due to compression or irritation of spinal nerves.
8. Grinding or popping sounds: Some people may experience clicking, grinding, or popping sounds (crepitus) when moving their neck. This is due to the wear and tear on the cervical spine.
9. Difficulty swallowing: In rare cases, cervical spondylosis may cause difficulty in swallowing (dysphagia) if there is pressure on the esophagus.
It’s important to note that not everyone with cervical spondylosis will experience all of these symptoms, and the severity of symptoms can vary. Suppose you suspect you have cervical spondylosis or are experiencing persistent neck pain or related symptoms. In that case, it is advisable to contact a healthcare professional for an accurate diagnosis & appropriate management.
Treatment Of Cervical Spondylosis
Many people wonder how to cure cervical spondylosis permanently, especially if they experience chronic or severe symptoms that affect their quality of life. While there is no definitive cure for cervical spondylosis, there are several treatment options available that can help manage the condition & limit further damage to the spine. The treatment plan depends on the severity of the symptoms, the extent of the degeneration, and the individual’s preferences and goals.
The primary goal of treatment is to relieve pain, reduce inflammation, improve mobility and function, & restrict long-term injury to the spinal cord and nerves. Some of the common treatments are:
– Medications: These include painkillers, anti-inflammatory drugs, muscle relaxants, & nerve pain medications. They can help reduce pain & inflammation, but they may have side effects such as stomach upset, drowsiness, or addiction.
– Physical therapy: This involves exercises, stretches, massage, heat therapy, cold therapy, electrical stimulation, and ultrasound. They can help improve the flexibility, strength, and mobility of the neck and spine. They can also reduce pain and prevent further deterioration of the spine.
– Lifestyle changes: These include avoiding activities that worsen the symptoms, such as lifting heavy objects, bending or twisting the neck, or using a phone or computer for long periods. They also include improving posture, sleeping on a firm mattress and pillow, using ergonomic furniture and equipment, and managing stress.
– Alternative therapies: These include acupuncture, chiropractic care, yoga, meditation, herbal remedies, and supplements. They can help relieve pain and improve well-being, but they may not be scientifically proven or regulated.
– Surgery: This is usually considered a last resort when other treatments fail to provide relief or when there is serious harm to the spinal cord or nerve roots. Surgery involves removing the damaged or degenerated parts of the spine and fusing the vertebrae with metal plates, screws, rods, or cages. Surgery can help restore the stability and alignment of the spine and relieve pressure on the spinal cord or nerve roots. However, surgery has risks such as infection, bleeding, nerve damage, spinal fluid leakage, or failure of fusion.
The cost of cervical spondylosis treatment in India differs depending on the type of treatment chosen, the hospital or clinic where it is done, the doctor who performs it, and the city where it is located. The following table gives an approximate range of costs for some common treatments in India:
| Treatment | Cost Range (INR) |
| Medications | 500 – 5,000 per month |
| Physical therapy | 2,000 – 5,000 per session |
| Lifestyle changes | No direct cost |
| Alternative therapies | 500 – 10,000 per session |
| Surgery | 2.4 lakhs – 5.4 lakhs |
The cost of surgery may vary depending on the type of surgery performed. For example:
– Cervical fusion (with implant): This involves fusing two or more vertebrae with an artificial disc or bone graft. The cost may range from 2.4 lakhs to 3.6 lakhs.
– Discectomy: This involves removing a herniated or bulging disc that presses on a nerve root. The cost may range from 3.6 lakhs to 5.8 lakhs.
– Spinal disc replacement: This involves replacing a damaged disc with an artificial one that mimics its function. The cost may range from 3.9 lakhs to 7.5 lakhs.
The cost of surgery may also include other expenses such as hospital stay, anesthesia charges, diagnostic tests, medications, physiotherapy sessions, post-operative consultation, and follow-up care. These may add up to another 1 lakh to 2 lakhs.
Therefore, the total cost of cervical spondylosis treatment in India may range from a few thousand rupees for conservative treatments to several lakhs for surgical treatments. However, the cost should be one of many factors to consider when choosing a treatment option. The effectiveness, safety, and suitability of the treatment for the individual patient should also be taken into account.
In addition to the treatment choices mentioned above, some self-care measures can help prevent or manage cervical spondylosis. These include:
– Maintaining a healthy weight: Being overweight can put more strain on the neck joints and discs and worsen cervical spondylosis. Therefore, it is important to keep a healthy weight by following a proper diet & exercising regularly.
– Avoiding activities that aggravate symptoms: Certain activities, like lifting heavy objects, holding the phone between the ear and shoulder, or working on a computer for long hours, can increase stress on the neck and worsen cervical spondylosis. Therefore, it is advisable to avoid these activities or modify them by using proper techniques or equipment.
– Applying heat or cold: Applying a warm compress or an ice pack to the neck can help reduce pain and inflammation caused by cervical spondylosis. Heat can relax muscles & improve blood flow, while cold can numb nerves and reduce swelling. However, care should be taken not to apply heat or cold straight to the skin or for more than 15 minutes at a time.
– Taking breaks: Taking frequent breaks from sitting or standing in one position can help avoid stiffness and soreness in the neck. It is recommended to change positions every 20 minutes and stretch gently.
– Sleeping well: Getting enough sleep can help heal damaged tissues and reduce inflammation in the neck. It is also important to use a comfortable pillow and mattress that support the natural curve of the neck.
– Quitting smoking: Smoking can impair blood circulation and oxygen delivery to the spine, which can delay healing and worsen cervical spondylosis. Therefore, quitting smoking can improve spinal health and overall well-being.
Cervical spondylosis is a common and progressive medical condition that can cause pain & disability in the neck. While there is no enduring cure for cervical spondylosis, several treatment options are available that can help manage the symptoms & prevent complications. The best treatment plan depends on the individual’s condition and preferences. By following the doctor’s advice and taking care of oneself, one can live a comfortable and productive life with cervical spondylosis.
Cervical Spondylosis Meaning
Cervical spondylosis is a term that describes the changes that happen in the neck (cervical) spine as people get older. It is a type of arthritis that affects the discs, joints, ligaments, and bones of the neck. These structures can wear out over time due to aging, injury, overuse or other factors.
Cervical spondylosis is very common and affects most people over the age of 60. It may not cause any symptoms in some people, but in others, it can cause pain, stiffness, numbness, tingling, weakness, or loss of balance. Sometimes, cervical spondylosis can also compress the spinal cord or nerve roots in the neck, leading to more serious problems.
There is no cure for cervical spondylosis, but there are medical therapies that can help relieve the symptoms and prevent further damage. These treatments may include medication, physical therapy, surgery or lifestyle changes. Some of the things that can help prevent or manage cervical spondylosis are:
– Maintaining good posture and avoiding neck strain
– Doing exercises to strengthen and stretch the neck muscles
– Taking anti-inflammatory drugs or muscle relaxants as prescribed
– Quitting smoking and maintaining a healthy weight
– Seeking medical attention if symptoms are serious or persistent
Cervical spondylosis is a common medical condition that affects the quality of life of many people. By understanding its meaning, causes, symptoms, and treatments, you can take steps to safeguard your neck & improve your well-being.
Cervical Spondylosis Causes
Several factors contribute to the development of cervical spondylosis, and these causes often interact with each other. Here are some factors that can contribute to cervical spondylosis:
1. Age:
– Cervical spondylosis is commonly associated with aging. As people get older, the spinal discs, which act as cushions between the vertebrae, tend to lose water content and elasticity. This makes them more susceptible to wear and tear, leading to degeneration.
2. Disc Degeneration:
– The intervertebral discs in the cervical spine change over time. These discs can degenerate due to a reduction in water content and structural alterations. Disc degeneration can lead to a decrease in disc height, leading to changes in the alignment and stability of the spine.
3. Bone Spurs (Osteophytes):
– As a response to the degeneration of the intervertebral discs, the body may form bone spurs (osteophytes). These are bony projections that can develop along the edges of the vertebrae. Bone spurs can narrow the space available for nerve roots and the spinal cord, causing compression and leading to symptoms like pain and numbness.
4. Genetic Factors:
– Genetic factors can play a vital part in the development of cervical spondylosis. Some people may be genetically predisposed to have a higher risk of developing degenerative spine conditions.
5. Occupational and Lifestyle Factors:
– Certain occupations and lifestyle choices may contribute to cervical spondylosis. Jobs or activities that involve repetitive neck motions, heavy lifting, or persistent periods of sitting in poor posture can increase the risk. Smoking and lack of regular exercise may also be related to a higher likelihood of getting cervical spondylosis.
6. Injury and Trauma:
– Past neck injuries, such as fractures or dislocations, can increase the risk of cervical spondylosis. Trauma may accelerate the degenerative process in the spine.
7. Obesity:
– Excess body weight can lead to increased stress on the cervical spine. The additional load on the neck can lead to faster degeneration of the spinal structures.
8. Medical Conditions:
– Certain medical conditions, like rheumatoid arthritis or spinal infections, may contribute to the development of cervical spondylosis.
How Is Cervical Spondylosis Diagnosed?
To confirm the diagnosis & rule out other causes of your symptoms, your physician may order some imaging tests. These tests can show the details of your cervical spine and reveal any abnormalities such as bone spurs, disc herniation, spinal stenosis, or spinal cord compression. The most common imaging tests for cervical spondylosis are:
– Neck X-ray: This test uses radiation to produce images of your neck bones. It can show changes in the shape and alignment of your vertebrae, such as narrowing of the disc spaces or formation of bone spurs.
– Magnetic resonance imaging (MRI): This test uses a strong magnetic field & radio waves to create comprehensive images of your soft tissues, such as your spinal cord and nerve roots. It can show if there is any pressure on your spinal cord or nerves from disc herniation, bone spurs, or spinal stenosis.
– Computed tomography (CT) myelography: This test combines a CT scan with an injection of a dye into your spinal canal. The dye highlights certain areas of your spine and makes it easier to see the details of your spinal cord and nerve roots. This test is usually done if an MRI is not available or is not suitable for you.
In some cases, your doctor may also order some nerve function tests to measure how well your nerves are transmitting signals to your muscles. These tests can help determine if you have cervical radiculopathy or nerve damage from cervical spondylosis. The most common nerve function test is:
– Electromyography (EMG): This diagnostic test measures the electrical activity in your nerves and muscles when they contract and relax. It involves inserting thin needles into your muscles and applying small shocks to stimulate your nerves.
– Nerve conduction study (NCS): This test measures the speed and strength of signals traveling through your nerves. It involves attaching electrodes to your skin above the nerve to be tested and applying small shocks to stimulate the nerve.
The results of these diagnostic tests will help your doctor diagnose cervical spondylosis and plan your treatment options.
Outlook / Prognosis Of Cervical Spondylosis
The outlook or prognosis of cervical spondylosis depends on several factors, such as:
– The severity and progression of the condition
– The response to treatment
– The presence of complications
– The individual’s age and general health.
In general, most people with cervical spondylosis have some long-term symptoms that may improve with nonsurgical treatment and do not need surgery. Many people with this condition are able to maintain an active life with some modifications and precautions. Some people may have to live with chronic pain that affects their daily activities and well-being.
Complications Of Cervical Spondylosis
Cervical spondylosis is commonly associated with aging and can lead to various complications. Here are some potential complications of cervical spondylosis:
1. Neck pain & stiffness: The most common symptom of cervical spondylosis is neck pain and stiffness. This can affect the quality of life and restrict the scope of motion in the neck.
2. Radicular symptoms: As cervical spondylosis progresses, it may lead to compression of nerve roots, resulting in radicular symptoms. This can result in pain, tingling, or numbness that radiates down the arms and into the hands.
3. Cervical radiculopathy: Compression of nerve roots in the cervical spine can lead to cervical radiculopathy, which may cause weakness, numbness, and pain in the shoulders, arms, and hands.
4. Myelopathy: In severe cases, cervical spondylosis can lead to compression of the spinal cord, known as cervical myelopathy. This can result in symptoms such as difficulty walking, coordination problems, and muscle weakness.
5. Loss of bladder or bowel control: Rarely, advanced cervical spondylosis can lead to serious complications such as loss of bladder or bowel control. This is a medical emergency & requires immediate attention.
6. Degenerative Disc Disease (DDD): Cervical spondylosis can contribute to the development of degenerative disc ailment, where the intervertebral discs in the neck decay over time, causing further pain and discomfort.
7. Spinal stenosis: The narrowing of the spinal canal, known as spinal stenosis, can occur with cervical spondylosis. This can put pressure on the spinal cord and nerves, leading to various neurological symptoms.
8. Reduced quality of life: Chronic pain and functional limitations associated with cervical spondylosis can have a high impact on an individual’s quality of life, influencing their ability to perform daily activities and engage in recreational or occupational pursuits.
It’s important to note that not everyone with cervical spondylosis will experience all of these complications, and the severity of symptoms can vary.
Conclusion
In conclusion, understanding cervical spondylosis is crucial for early detection and effective management of this common neck condition. Recognizing the symptoms, such as neck pain, stiffness, and headaches, is key to seeking timely medical attention. Fortunately, a range of treatments is available, encompassing conservative approaches such as physical therapy, medication, & lifestyle modifications, as well as more invasive options like surgery in severe cases. By adopting a holistic approach to care, anyone can mitigate symptoms, improve their quality of life, and maintain neck health in the face of cervical spondylosis.
Cervical spondylosis treatment can involve a range of medical expenses, including diagnostic tests, medications, physiotherapy, and, in severe cases, surgery. Many individuals in India face financial constraints that limit their ability to access the necessary healthcare. A crowdfunding platform can bridge this gap by enabling people to raise funds collectively, making treatment more financially accessible.












