In the ever-evolving landscape of medical science, hope shines brightest when it comes to groundbreaking treatments for life-threatening diseases. One such innovation that has stirred the global medical community is CAR T cell therapy. This cutting-edge approach to cancer treatment has transcended boundaries and is now making its mark in India, offering renewed optimism to those battling cancer. In this blog, we delve into the fascinating world of CAR T cell therapy in India, exploring what it is, how it works, and its growing impact on the healthcare system.
Cancer remains one of the most formidable adversaries in the field of medicine, affecting millions of lives worldwide. Traditionally, the approach to treating cancer has involved surgery, chemotherapy, and radiation therapy. However, these methods have limitations, and the quest for more effective & less invasive treatment options continues. This is where CAR T cell therapy steps in, offering a promising alternative for patients in India and beyond.
What sets CAR T cell therapy apart is its personalized and highly targeted approach. Unlike traditional cancer treatments, CAR T cell therapy tailors the treatment to each patient’s unique genetic makeup, allowing for a more precise attack on cancer tumors while minimizing harm to healthy tissues. This revolutionary approach has shown remarkable results, particularly in people with certain kinds of blood cancers like leukemia and lymphoma.
The emergence of CAR T cell therapy in India is a significant development in the country’s healthcare landscape. Over the past few years, several healthcare institutions and research centers have embraced this innovative treatment, bringing hope to many cancer patients who may have exhausted conventional options. The availability of CAR T cell therapy in India reduces the need for patients to seek treatment abroad and contributes to the nation’s medical expertise.
In this article, we will find the science behind CAR T cell therapy, its application in India, the challenges and opportunities it presents, and the transformative impact it has on cancer care. By understanding the intricacies of this cutting-edge therapy, we hope to shed light on the promising future it holds for cancer patients in India and worldwide. Join us on this journey through CAR T cell therapy, where science, innovation, and compassion converge to redefine the boundaries of cancer treatment.
Table of Contents
CAR T Cell Therapy Cost In India
But this scenario is about to change soon. India is on the verge of launching its own homegrown CAR T-cell therapy that will be more affordable and accessible for Indian patients. Mumbai-based Immunoadoptive Cell Therapy Private Limited (ImmunoACT), an IIT Bombay-incubated company has announced the approval of India’s first indigenously developed CD19-targeted CAR T-cell therapy by the CDSCO on October 13, 2023. CD19 is a biomarker for B lymphocytes & can be used as a mark for leukemia immunotherapies.
The therapy, called NexCAR19, has been developed in collaboration with Tata Memorial Hospital in Mumbai, where clinical trials were conducted with 60 patients with relapsed or refractory B-cell lymphomas and leukemia. The clinical data indicated a 70% overall response rate, which means that 70% of the patients showed some degree of improvement after the therapy. The therapy also showed a low toxicity profile, with minimal side effects such as cytokine release syndrome (CRS), a common complication of CAR T-cell therapy that causes fever, low blood pressure, and organ damage.
The most remarkable feature of NexCAR19 is its cost-effectiveness. The therapy will be available at 20 Indian government and private hospitals treating cancer across significant cities at around Rs 30-35 lakh per patient. This is about 10 times cheaper than the cost of CAR T-cell therapy in the US. This price difference is because ImmunoACT has developed its technology platform for producing CAR T-cells in India, which reduces dependence on foreign companies and laboratories.
ImmunoACT is not the only company working on CAR T-cell therapy in India. Other companies such as Cellogen Biosciences, Immuneel Therapeutics, and Actrec have also initiated clinical trials for their versions of CAR T-cell therapy for different types of cancers. These trials are expected to be completed by early 2024, after which these therapies will be available commercially in India. These therapies are expected to cost as low as $20,000 per patient.
Car T cell therapy is a breakthrough in cancer treatment that has shown remarkable results in patients with blood cancers like leukemia & lymphoma. India has made a significant achievement by approving its first indigenous Car T cell therapy product, NexCAR19, which will provide access to this cutting-edge treatment at an affordable cost. However, there is still a need for more research and development to overcome the challenges and limitations of this therapy and to expand its applicability to other types of cancers.
Factors Affecting The CAR T Cell Therapy Cost In India
The cost of CAR T-cell therapy in India, as in other countries, can vary significantly based on several factors. CAR T-cell therapy is a highly personalized and complex treatment that involves modifying a patient’s T cells to target cancer cells. Here are some of the key factors that can affect the cost of CAR T-cell therapy in India:
1. Type of Cancer: The type of cancer being treated can significantly impact the cost. CAR T-cell therapy is currently approved for certain types of blood cancers, like B-cell acute lymphoblastic leukemia (B-ALL) & diffuse large B-cell lymphoma (DLBCL). The specific cancer and its stage will affect the treatment approach and cost.
2. Hospital or Treatment Center: The choice of hospital or treatment center can greatly influence the cost. Premier hospitals and specialized cancer centers may charge more for CAR T-cell therapy due to their advanced facilities, experienced medical staff, and better amenities.
3. CAR T-cell Product: The specific CAR T-cell product can cost differently. Various pharmaceutical companies may develop these products and have other pricing structures.
4. Pre-Treatment Workup: The cost includes pre-treatment evaluations and tests to assess the patient’s eligibility and prepare them for CAR T-cell therapy. This may include genetic testing, imaging, and other diagnostic tests.
5. Cell Collection and Processing: The process of collecting the patient’s T cells, modifying them to express chimeric antigen receptors (CARs), and expanding them in the laboratory can be a labor-intensive and expensive step in the treatment.
6. Hospital Stay: The length of hospitalization and the associated costs can differ depending on the patient’s response to treatment and any potential side effects.
7. Follow-Up Care: Post-treatment care, including monitoring and any necessary interventions, can add to the overall cost.
8. Geographic Location: The cost of healthcare services in India can vary by region, so the location of the treatment center can impact the overall cost.
9. Insurance Coverage: Health insurance coverage, if available, can help mitigate out-of-pocket expenses for patients. However, not all insurance plans cover CAR T-cell therapy, and coverage terms may vary.
10. Government Regulations and Approvals: Regulatory approvals and pricing regulations set by the government can influence the cost of CAR T-cell therapy.
11. Research and Development Costs: The cost of CAR T-cell therapy may also reflect the research and development expenses associated with creating and improving these treatments.
It’s necessary to consult with a medical professional and the treatment center to get a precise estimate of the cost based on your specific condition and treatment plan.
What Is CAR T Cell Therapy?
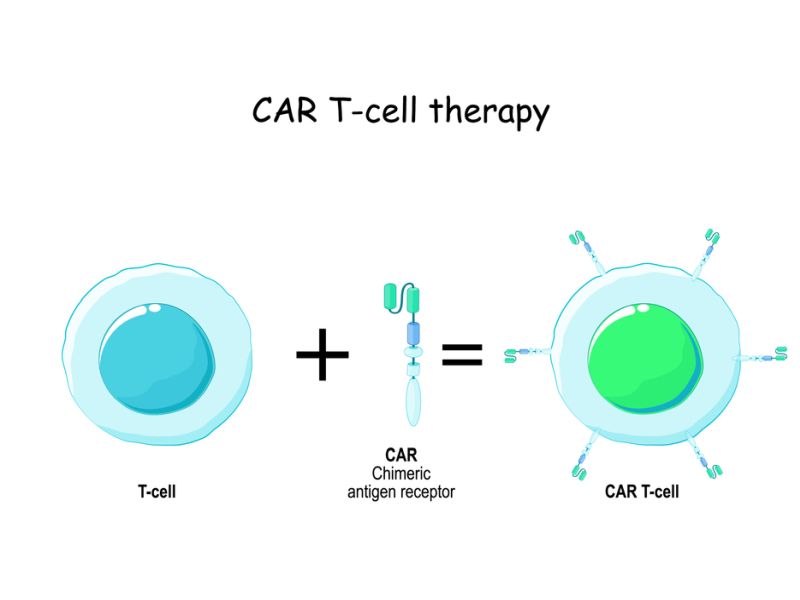
Chimeric Antigen Receptor T-cell therapy, commonly known as CAR T-cell therapy, is an innovative and highly specialized form of immunotherapy used to treat certain types of cancer. It’s a revolutionary approach that harnesses the power of a patient’s own immune system to target and destroy cancer cells.
Here’s how CAR T-cell therapy works:
1. Collection of T Cells: First, a patient’s T cells are collected through leukapheresis. These T cells play an important role in the immune system’s ability to fight infections & diseases.
2. Genetic Modification: The collected T cells are genetically engineered in a laboratory. This involves the insertion of a synthetic gene into the T cells, which encodes a chimeric antigen receptor (CAR). This receptor is built to recognize a specific protein found on the surface of cancer tumors.
3. Expansion and Activation: The modified T cells are grown and multiplied in the laboratory until there is a sufficient quantity of CAR T cells. During this process, the CAR T cells are also activated to enhance their ability to target cancer cells.
4. Infusion: The patient undergoes a process known as lymphodepletion, which involves the depletion of some of the patient’s existing immune cells. This creates a more favorable environment for the infused CAR T cells. After lymphodepletion, the engineered CAR T cells are infused back into the patient’s bloodstream.
5. Targeting and Destruction: Once inside the patient’s body, the CAR T cells can recognize the specific cancer antigen they were designed to target. When they encounter cancer cells with that antigen, they become activated and attack the cancer cells, destroying them.
CAR T-cell therapy has shown exceptional success in treating certain kinds of blood cancers, like acute lymphoblastic leukemia (ALL) and some forms of non-Hodgkin lymphoma. The therapy has demonstrated impressive response rates in patients who have exhausted other treatment options. However, it is a complex and sometimes challenging treatment associated with potential side effects, including cytokine release syndrome and neurologic toxicities. Patients receiving CAR T-cell therapy are closely monitored and managed by healthcare professionals with experience in the field.
Types Of Cancer Treated With CAR T Cell Therapy
Currently, CAR T cell therapy has been accepted by the Food & Drug Administration (FDA) in the United States for treating certain types of blood cancers that affect B cells. B cells are another white blood cell type that produces antibodies to fight infections. However, sometimes B cells can become cancerous and form tumors called lymphomas or leukemias.
The FDA has approved four CAR T cell therapies for treating specific B cell cancers in certain groups of patients:
– Breyanzi: Suitable for adults with relapsed or refractory large B cell lymphoma
– Tecartus: Option for adults with relapsed or refractory mantle cell lymphoma
– Kymriah: for children & young adults up to 25 years old with acute lymphoblastic leukemia (ALL) and adults with relapsed large B cell lymphoma
– Yescarta: Suitable for adults with relapsed or refractory large B cell lymphoma
These CAR T cell therapies target an antigen called CD19, which is found in most B-cell cancers. However, not all B cell cancers have CD19, and some cancers may lose CD19 over time or develop resistance to CAR T cell therapy. Therefore, scientists are developing new CAR T cell therapies that target other antigens, such as CD20, CD22, or BCMA.
Scientists are also investigating whether CAR T cell therapy can effectively treat other types of cancer, such as solid tumors (cancers that form masses in organs or tissues). Some examples of solid tumors that are being studied for CAR T cell therapy include:
– Brain tumors
– Breast cancer
– Colorectal cancer
– Lung cancer
– Ovarian cancer
– Prostate cancer
However, treating solid tumors with CAR T cell therapy poses more challenges than treating blood cancers. For instance, solid tumors may have more diverse antigens than blood cancers, making it harder to find a single target for CAR T cells. Solid tumors may also have more barriers that prevent CAR T cells from reaching them, such as low blood supply or high pressure. Moreover, solid tumors may have more mechanisms that suppress or evade the immune system, such as producing immunosuppressive molecules or hiding their antigens.
Therefore, more research is needed to overcome these obstacles and optimize CAR T cell therapy for solid tumors.
Benefits Of CAR T-Cell Therapy
The main benefit of CAR T-cell therapy is that it can be very effective for people with blood cancers who do not respond to other treatments, like chemotherapy or stem cell transplant. CAR T-cell therapy can offer a chance of cure or long-term remission for some people who have no other options.
According to clinical trials and real-world data, CAR T-cell therapy has shown impressive results for some types of blood cancers, such as:
– B-cell acute lymphoblastic leukemia (ALL), a cancer affecting not fully grown white blood cells in the bone marrow. In a trial of children and young adults with relapsed or refractory ALL who received tisagenlecleucel (Kymriah), a type of CAR T-cell therapy, 81% achieved complete remission within three months of treatment.
– B-cell non-Hodgkin lymphoma (NHL) is a group of cancers affecting mature white blood cells in the lymph nodes and other organs. In a trial of adults with relapsed or refractory large B-cell lymphoma who received axicabtagene ciloleucel (Yescarta), another type of CAR T-cell therapy, 51% achieved complete remission within two months of treatment.
– Multiple myeloma is a kind of cancer affecting plasma cells in the bone marrow. In a trial of adults with relapsed or refractory multiple myeloma who received idecabtagene vicleucel (Abecma), yet another type of CAR T-cell therapy, 28% achieved complete remission within six months of treatment.
Another benefit of CAR T-cell therapy is that it can be personalized for each patient. Unlike conventional drugs made for everyone, CAR T-cells are made from your own cells and tailored to target your specific cancer. This can increase the chances of success and reduce the risk of side effects.
Additionally, CAR T-cell therapy can be a one-time treatment with lasting effects. Unlike chemotherapy or other drugs that must be taken repeatedly, CAR T-cell therapy can provide a single infusion that can keep working for months or years. Some studies have shown that CAR T-cells can persist in the body and provide long-term protection against cancer recurrence.
CAR T-Cell Therapy Side Effects
While CAR T-cell therapy can effectively eliminate cancer cells, it is associated with some potentially severe side effects. These side effects can differ in severity & onset, and they are typically referred to as cytokine release syndrome (CRS) and neurologic toxicity. Here are some of the common side effects associated with CAR T-cell therapy:
1. Cytokine Release Syndrome (CRS): CRS is one of CAR T-cell therapy’s most common and potentially severe side effects. It occurs when the CAR T-cells are activated and release many cytokines (proteins that regulate the immune response). Symptoms of CRS can vary from mild to severe and may include fever, chills, nausea, vomiting, diarrhea, low blood pressure, and difficulty breathing. Severe cases of CRS can lead to organ dysfunction and require intensive medical management.
2. Neurologic Toxicity: Neurologic toxicity, also known as CAR T-cell-related encephalopathy syndrome (CRES), can cause confusion, delirium, seizures, and other neurological symptoms. The exact cause of neurologic toxicity is poorly understood, but it is thought to result from an excessive immune response in the central nervous system.
3. Cytopenias: Some patients may experience decreased blood cell counts, which include red blood cells, white blood cells, & platelets. This can lead to anemia, infections, & bleeding issues.
4. Infections: CAR T-cell therapy can weaken the immune system, making patients more easily affected by infections. Patients receiving CAR T-cell therapy are often monitored closely for signs of infection and may receive prophylactic antibiotics.
5. Hypotension: Low blood pressure can occur due to CRS, which can be serious and requires careful monitoring and intervention.
6. Hepatotoxicity: Some patients may experience liver inflammation and damage, leading to elevated liver enzymes. This can be monitored through blood tests.
7. Pulmonary Toxicity: Lung-related complications, such as pulmonary edema or respiratory distress, can occur as a result of CRS.
8. Tumor Lysis Syndrome: In some cases, the rapid destruction of cancer cells by CAR T-cells can lead to the release of cellular contents into the bloodstream. This can overload the kidneys and cause metabolic disturbances.
9. Cardiac Complications: While less common, CAR T-cell therapy can lead to cardiac complications, including arrhythmias and decreased cardiac function.
It’s important to note that the severity of these side effects can differ from patient to patient. Careful monitoring and management by healthcare providers are crucial during and after CAR T-cell therapy. Patients and their families should receive detailed information about potential side effects and what to watch for during treatment. Patients considering CAR T-cell therapy should discuss the potential risks & benefits with their healthcare team.
How Is The Recovery Process After CAR T Cell Therapy?
The recovery process after CAR T cell therapy varies depending on the type and severity of side effects and complications. Patients may need to stay in the hospital for several days or weeks after CAR T cell infusion to monitor their condition and treat any adverse reactions. Patients may also need to take medications to prevent or manage infections, CRS, neurologic toxicity, B cell aplasia, or TLS.
Patients may need regular blood tests and scans to check their response to CAR T cell therapy and overall health. Patients may also need to have follow-up infusions of CAR T cells if the cancer comes back or does not respond completely.
Patients should avoid live vaccines for at least 6 weeks after CAR T cell therapy, as they may cause serious infections. Patients should also avoid pregnancy for at least 12 months after CAR T cell therapy, as it may harm the fetus.
Patients should consult their doctor before starting or stopping any medications or supplements after CAR T cell therapy. Patients should also report any new or worsening symptoms to their doctor immediately.
Conclusion
In conclusion, CAR T cell therapy in India represents a revolutionary and promising breakthrough in the field of cancer treatment. This innovative approach harnesses the power of a patient’s immune system to combat cancer, offering new hope to individuals battling various forms of the disease.
One of the significant advantages of CAR T cell therapy in India is its accessibility and affordability. The country has emerged as a center for medical tourism, attracting patients from everywhere around the world seeking top-notch healthcare at a fraction of the price in Western countries. Indian hospitals and medical facilities have been quick to adopt this cutting-edge therapy, making it accessible to a broader patient population.
Furthermore, the government’s efforts to streamline regulations and expedite approvals for CAR T cell therapy have created a conducive environment for its growth in the country. This means that more patients in India can benefit from this groundbreaking treatment option.
In summary, CAR T cell therapy in India represents a beacon of hope for cancer patients and a cost-effective and accessible solution. With the rapidly advancing medical infrastructure and regulatory support, the future of CAR T cell therapy in India looks promising, offering renewed chances of recovery and improved quality of life for those touched by the scourge of cancer.
CAR T Cell Therapy is often expensive, making it unaffordable for many. Crowdfunding can help ease the financial burden by allowing individuals to raise funds for their treatment. It democratizes access to medical care.












