Wilson Disease, a rare genetic disorder, is characterized by the unusual accumulation of copper in various body organs, particularly the liver, brain, and other tissues. This condition is named after Dr. Samuel Alexander Kinnier Wilson, who first described it in 1912. Understanding the intricacies of Wilson Disease is crucial for early detection, proper management, and improved outcomes for affected individuals.
The clinical presentation of Wilson’s Disease can vary widely, making diagnosis challenging. Common signs include liver-related symptoms such as jaundice, abdominal pain, and hepatomegaly. Neurological symptoms such as tremors, difficulty speaking, and impaired coordination may also manifest. Additionally, psychiatric symptoms like mood swings, depression, and cognitive impairment may be present. Recognizing these diverse manifestations is crucial for timely intervention and effective treatment.
Wilson Disease is an autosomal recessive hereditary disease caused by mutations in the ATP7B gene responsible for regulating copper transport within the body. Usually, this gene facilitates the incorporation of copper into ceruloplasmin, a protein that transports copper in the blood. In Wilson Disease, dysfunctional ATP7B leads to impaired copper transport, resulting in its accumulation within various tissues. Genetic testing is crucial for assuring the diagnosis & identifying carriers of the faulty gene.
Diagnosing Wilson Disease involves a comprehensive approach, combining clinical evaluation, laboratory tests, and imaging studies. Liver function tests, serum ceruloplasmin levels, and 24-hour urinary copper excretion are commonly used to assess copper metabolism. Molecular genetic testing can affirm the presence of ATP7B mutations. Additionally, imaging techniques like liver biopsy and radiological studies aid in evaluating the extent of organ damage.
Managing Wilson’s Disease necessitates a multifaceted approach to reduce copper accumulation and alleviate symptoms. Chelating agents, like penicillamine and trientine, facilitate copper excretion in the urine. Zinc supplements may be prescribed to inhibit copper absorption in the digestive tract. In serious cases, liver transplantation may be considered as a life-saving intervention. Close monitoring and lifelong treatment adherence are crucial to prevent disease progression and complications.
Wilson Disease poses significant challenges in terms of diagnosis and management, underscoring the importance of increased awareness among healthcare professionals and the general public. Early detection, genetic counseling, and advances in treatment modalities have improved the prognosis for individuals with Wilson Disease.
Table of Contents
Wilson Disease Symptoms
Wilsons disease symptoms is a rare disease that causes copper to accumulate in various organs of the body. The underlying cause is a mutation in the ATP7B gene, which regulates the transport of copper in the body. This results in the impaired ability to excrete excess copper, leading to its accumulation in different tissues and organs. Copper is essential for various bodily functions, but excess copper can be toxic.
Here’s an overview of how Wilson’s disease affects different body organs and the associated symptoms:
1. Liver:
– Wilson’s disease primarily affects the liver due to the defective ATP7B gene, impairs the liver’s ability to transport copper into the bile for excretion. Instead, copper accumulates in the liver cells.
– In the early stages, individuals may experience nonspecific symptoms like fatigue, weakness, and abdominal pain.
– As copper builds up, hepatocellular apoptosis occurs, leading to inflammation and liver damage.
– Over time, hepatomegaly (enlarged liver) may occur.
– Jaundice, a yellowing of the skin and eyes, can occur due to impaired liver function.
– In severe cases, cirrhosis may develop, increasing the risk of liver failure.
2. Central Nervous System:
– Copper accumulation in the central nervous system contributes to neurological symptoms.
– Tremors, particularly in the hands, can be an early sign. These tremors may resemble those seen in Parkinson’s disease.
– Ataxia, or impaired coordination, is common. It can affect balance and gait.
– Dysarthria, a difficulty in articulating words, may be present.
– Dystonia, characterized by involuntary muscle contractions, can occur, leading to abnormal postures.
3. Cornea:
– Copper deposits in the cornea of the eyes result in the formation of Kayser-Fleischer rings. These are greenish-brown rings encircling the cornea.
– Kayser-Fleischer rings are caused by copper deposition in Descemet’s membrane and are a key diagnostic feature.
– While they don’t typically affect vision, their presence is vital for diagnosing Wilson’s disease.
4. Kidneys:
– Copper buildup in the kidneys is less common but can lead to renal complications.
– Kidney involvement may result in impaired function, influencing the organ’s ability to refine waste from the blood.
5. Other Organs:
– Copper can accumulate in other organs, including the heart and lungs, but these manifestations are less common and less well-studied.
– In the heart, copper deposition might lead to cardiomyopathy (disease of the heart muscle).
– In the lungs, copper buildup may cause respiratory symptoms.
6. Psychiatric Symptoms:
– Wilson’s disease can also affect mental health. Psychiatric symptoms may include mood swings, depression, anxiety, and, in severe cases, psychosis.
– The exact mechanisms by which copper affects mental health are not fully understood but may involve the impact on neurotransmitter function.
It’s important to note that the symptoms and severity of Wilson’s disease can vary widely among individuals. Diagnosis generally involves a combination of clinical evaluation, blood tests, urine tests, and imaging studies. Early detection & treatment are crucial for managing Wilson’s disease. Treatment often involves medications that help remove excess copper from the body, and, in severe cases, liver transplantation may be considered.
Wilson Disease Treatment
The treatment of Wilson’s disease aims to reduce the amount of copper in the body and prevent further organ damage. The main treatment options are:
– Chelation therapy: This involves taking oral medications that bind to copper and help remove it from the body through urine or feces. The most commonly used drugs are penicillamine and trientine. These drugs have to be taken for life and may cause side effects such as skin rashes, fever, joint pain, kidney problems, and neurological symptoms.
– Zinc therapy: This involves taking oral zinc supplements that block the absorption of copper from the intestines and increase its excretion in feces. Zinc therapy is usually used as a maintenance treatment after chelation therapy or as an alternative for patients who cannot tolerate chelation therapy. Zinc therapy may cause side effects such as nausea, vomiting, abdominal pain, and anemia.
– Dietary modification: This involves avoiding foods that are high in copper, like shellfish, liver, nuts, chocolate, mushrooms, and dried fruits. Patients should also avoid drinking water from copper pipes or using copper utensils or cookware.
– Liver transplantation: This is a medical procedure that substitutes the damaged liver with a healthy one from a donor. Liver transplantation is kept for patients who have severe liver failure or who do not respond to other treatments. Liver transplantation can cure Wilson disease, but it carries risks such as infection, rejection, bleeding, and complications from immunosuppressive drugs.
The cost of Wilson disease treatment in India varies depending on the type of treatment, the duration of treatment, the hospital charges, and other factors. The approximate costs are:
– Chelation therapy: Penicillamine costs Rs 500 to Rs 4000 monthly, depending on the dosage and brand. The cost of trientine was Rs 2.2 crore per annum when imported, but it has been reduced to Rs 2.2 lakh per annum after being manufactured indigenously.
– Zinc therapy: The cost of zinc supplements ranges from Rs 100 to Rs 500 monthly, depending on the dosage and brand.
– Dietary modification: The cost of dietary modification depends on the availability and affordability of low-copper foods in different regions of India.
– Liver transplantation: The cost ranges from around Rs 15 lakh to Rs 25 lakh, based on the hospital charges, donor availability, surgery complexity, and post-operative care.
Wilson disease is a severe but treatable condition that requires lifelong management and monitoring. Patients with Wilson disease can lead everyday lives if they follow their treatment regimen and regular check-ups. Early diagnosis & treatment can prevent irreversible damage to the organs and improve the quality of life of patients with Wilson disease.
What Is Wilson’s Disease?
Wilson’s disease is a rare disease that affects how your body handles copper. Copper is a metal that we need in small amounts for our health, but too much of it can be harmful. Normally, our liver filters out the excess copper and releases it into bile, a fluid that helps digestion. However, a faulty gene prevents this process from working properly in people with Wilson’s disease. As a result, copper accumulates in the liver, brain, eyes, and other organs, causing damage and various symptoms.
How Common Is Wilson Disease In India?
Wilson’s disease affects about one in 30,000 people globally, but the prevalence may vary depending on the region and the ethnic group. The exact incidence of Wilson disease in India is unknown, but some studies have estimated that it may be around one in 10,000 to 15,000 people. This means that there could be more than 80,000 people with Wilson disease in India, but many of them may be undiagnosed or misdiagnosed.
Wilson Disease Causes
Here’s a detailed explanation of the causes and factors contributing to Wilson’s disease:
1. Genetic Inheritance:
– Wilson’s disease is an autosomal recessive congenital disease, meaning an affected person must inherit a mutated copy of the ATP7B gene from both parents.
– Individuals who inherit only one mutated copy (carriers) generally do not develop the disease but can pass the mutated gene to their children.
2. ATP7B Gene Mutation:
– The ATP7B gene provides instructions for the synthesis of the ATP7B protein.
– This protein is essential for transporting copper within the body, including its absorption from the intestines, incorporation into ceruloplasmin (a copper-carrying protein), and excretion through bile.
– Mutations in the ATP7B gene produce a dysfunctional ATP7B protein or its absence, disrupting the normal copper transport processes.
3. Copper Accumulation:
– In individuals with Wilson’s disease, copper accumulates in the liver due to the impaired ability to transport copper from the liver cells into the bile.
– The excess copper is then released into the bloodstream and distributed to other organs, particularly the central nervous system, kidneys, and corneas of the eyes.
4. Liver Dysfunction:
– The liver is the prime organ that Wilson’s disease affects. Copper accumulation in the liver can cause hepatic symptoms such as hepatomegaly (enlarged liver), jaundice, and liver damage.
– In some cases, stored copper may be released into the bloodstream during periods of physiological stress (e.g., infection, pregnancy), exacerbating symptoms.
5. Neurological Manifestations:
– Copper accumulation in the central nervous system can lead to neurological symptoms such as tremors, dystonia, and psychiatric disturbances.
– If left untreated, the neurological damage can progress to severe conditions such as cognitive impairment and difficulty with movement.
6. Environmental Triggers:
– While Wilson’s disease is primarily a genetic disorder, environmental factors can sometimes influence the age of onset and severity of symptoms.
– Certain environmental factors, such as dietary copper intake, may exacerbate symptoms in individuals with Wilson’s disease.
It’s important to note that Wilson’s disease can present with various symptoms and severity, and early diagnosis & treatment are crucial for managing the condition effectively.
Wilson Disease Diagnosis
To diagnose Wilson disease, doctors use a combination of medical and family history, physical and eye exams, and tests. Some tests include:
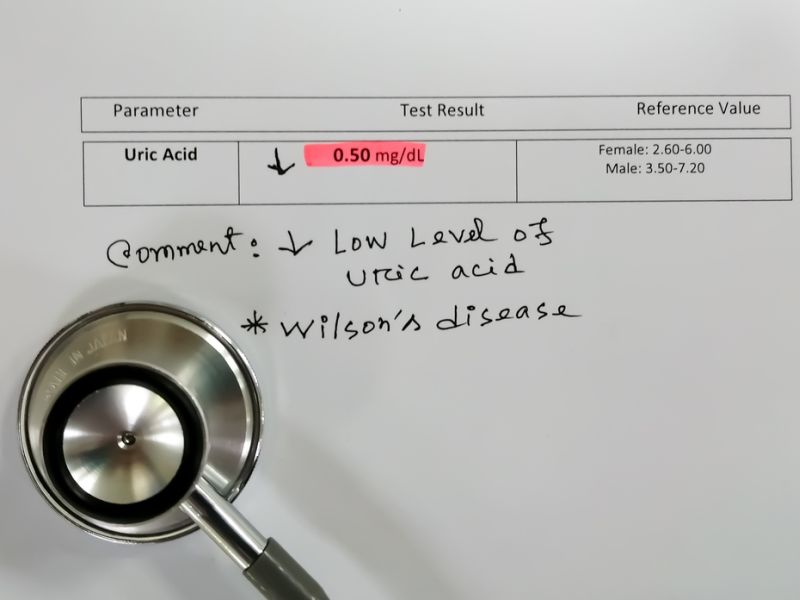
– Blood tests: These diagnostic tests measure the levels of ceruloplasmin, a protein that holds copper in the blood; copper liver enzymes; and red blood cells. People with Wilson disease often have low ceruloplasmin levels, lower than normal blood copper levels, abnormal liver enzyme levels, and signs of anemia. Blood tests can also check for the gene mutations that cause Wilson disease.
– Urine tests: They measure the amount of copper excreted in the urine during 24 hours. People with Wilson disease usually have higher than normal urine copper levels.
– Eye exam: This exam uses a special light to look for Kayser-Fleischer rings, brownish-green rings of copper deposits in the eyes. These rings are present in most people with Wilson disease.
– Liver biopsy: This procedure involves taking a small sample of liver tissue & examining it under a microscope for excess copper accumulation and signs of liver damage or cirrhosis. A liver biopsy can also measure the amount of copper in the liver tissue.
– Imaging tests: These tests use magnetic resonance imaging (MRI) or computed tomography (CT) scan to check for signs of Wilson disease or other conditions in the brain. Imaging tests are usually done for people who have nervous system symptoms.
The diagnosis of Wilson’s disease can be challenging because its symptoms are similar to other liver diseases and can vary from person to person. Also, some people with Wilson disease may not have any symptoms or abnormal test results until the disease progresses. Therefore, doctors may need multiple tests and criteria to confirm or rule out the diagnosis.
Wilson Disease Prognosis
The prognosis of Wilson’s disease depends on several factors, such as the age of onset, the severity of symptoms, the extent of organ damage, the response to treatment, and compliance with medication. If left untreated, Wilson’s disease can be fatal due to liver failure or neurological complications. The median life expectancy for untreated patients is 40 years.
However, if diagnosed early and treated properly, many people with Wilson disease can live normal lives with minimal or no symptoms. The life expectancy for treated patients may increase. Regular follow-up visits with a medical provider are important to monitor the condition & adjust the treatment as needed.
Risk Factors Of Wilson’s Disease
While the disease is genetic, not everyone with the mutation develops symptoms. Here are some risk factors associated with Wilson’s disease:
1. Genetic Factors:
– Wilson’s disease is a rare condition that happens when a person gets two copies of a changed gene, one from each parent.
– If both parents carry a single mutated copy of the ATP7B gene, there is a 25% chance that the child will inherit two mutated copies with each pregnancy and develop Wilson’s disease.
2. Family History:
– Having a family history of Wilson’s disease increases the risk. If a close relative, such as a parent or sibling, has Wilson’s disease, it raises the likelihood of other family members carrying the gene mutation.
3. Ethnicity:
– Wilson’s disease is found in individuals of all ethnic backgrounds, but it is more commonly diagnosed in people of Eastern European, Southern European, or Asian descent.
4. Age of Onset:
– Wilson’s disease symptoms often appear between the ages of 5 and 35, although they can manifest at any age. The age of onset may influence the severity of symptoms.
5. Gender:
– There is no significant gender difference in the occurrence of Wilson’s disease. Both males & females can be affected equally.
6. Liver Disease:
– Individuals with liver disease may be at a higher risk of complications from Wilson’s disease. The liver is a primary site of copper accumulation in this disorder, and pre-existing liver conditions may exacerbate the impact of copper overload.
7. Neurological Symptoms:
– Neurological symptoms may increase the risk of Wilson’s disease being identified, as they often lead to medical evaluation. Symptoms such as tremors, muscle stiffness, or coordination difficulty can indicate copper accumulation in the brain.
8. Delayed Diagnosis:
– A delay in diagnosis and treatment may contribute to the progression of Wilson’s disease and an increased risk of complications. Timely identification and intervention are crucial in managing the disorder effectively.
It’s important to note that while these factors can increase the likelihood of developing Wilson’s disease, not everyone with these risks will necessarily acquire the medical condition.
Complications Of Wilson’s Disease
Copper is essential for many physiological processes in the body, but in individuals with Wilson’s disease, there is a defect in the transport of copper, leading to its abnormal accumulation. This can result in various complications affecting different organ systems. Here are some complications associated with Wilson’s disease:
1. Liver Complications:
– Hepatitis: Copper buildup in the liver can cause inflammation, leading to hepatitis. As time goes by, the swelling in the liver can lead to cirrhosis, which is when the liver tissue gets scarred. It can result in impaired liver function.
– Liver Failure: In severe cases, the accumulation of copper in the liver can lead to liver failure. This can be life-threatening and may require liver transplantation.
2. Neurological Complications:
– Neuropsychiatric Symptoms: Copper buildup in the brain can lead to various neurological symptoms, including tremors, dystonia (involuntary muscle contractions), and difficulty with speech and coordination.
– Psychiatric Symptoms: Wilson’s disease can also manifest with psychiatric symptoms like depression, anxiety, personality changes, & even psychosis.
– Movement Disorders: Some individuals may experience movement disorders, including chorea, characterized by involuntary, jerky movements.
3. Hematological Complications:
– Anemia: Copper is involved in the formation of red blood cells. In Wilson’s disease, the build-up of copper can cause anemia because it hampers the production of red blood cells.
– Coagulopathy: Copper plays a role in blood clotting. Abnormal copper levels can lead to bleeding disorders or clotting abnormalities.
4. Renal Complications:
– Kidney Issues: Although less common, Wilson’s disease can affect the kidneys. Copper deposition in the kidneys may lead to renal dysfunction.
5. Ocular Complications:
– Kayser-Fleischer Rings: These are copper deposits in the cornea of the eye. They can be observed during a clinical examination and indicate copper overload in the body.
6. Joint Complications:
– Arthritis: Copper accumulation in the joints may lead to arthritis, causing pain and inflammation.
It’s important to note that the severity and combination of complications can vary widely among individuals with Wilson’s disease.
Conclusion
In conclusion, Wilson’s Disease emerges as a rare yet impactful genetic disorder, encompassing a spectrum of symptoms that intricately affect both the liver and the nervous system. The foundation of this condition rests in a genetic mutation that disrupts the delicate balance of copper metabolism within the body, accumulating copper in vital organs.
The primary approach to treating Wilson’s Disease revolves around copper chelation therapy, a method aimed at reducing copper levels in the body. This underscores the importance of patient compliance with prescribed medications and regular monitoring to ensure the efficacy of the treatment plan. For individuals with advanced liver damage or inadequate response to medical therapy, liver transplantation remains a viable option.
Despite progress in understanding and managing Wilson’s Disease, challenges persist regarding accessibility to specialized healthcare and general awareness. Education about the disease, its varied symptoms, and the significance of genetic testing is crucial for fostering early detection and improving patient outcomes.
In essence, Wilson’s Disease serves as a paradigm of the intricate interplay between genetics, metabolism, and organ function. Ongoing research efforts and medical advancements hold promise for improved diagnostic tools and targeted therapies, raising optimism for a better quality of life for those affected by this complex and rare genetic disorder. The combined efforts of healthcare professionals, researchers, & advocacy groups remain pivotal in addressing the multifaceted aspects of Wilson’s Disease and advancing its overall management.
Wilson’s Disease demands urgent and sustained medical attention, involving medications, regular monitoring, and sometimes even liver transplantation. The cost of these interventions can be exorbitant, placing immense strain on individuals and families already grappling with the emotional & physical toll of the disease. A crowdfunding platform allows individuals to rally support from their communities, both near and far. Friends, family, and even strangers who empathize with the cause can contribute, creating a collective effort to alleviate the financial burden.












