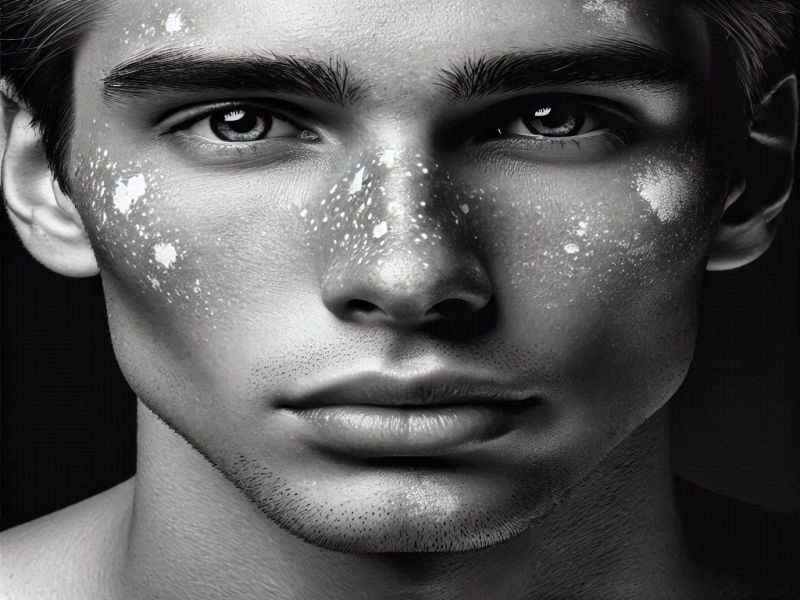
Have you ever noticed small white spots on your skin, disrupting the smooth canvas of your natural tone? These seemingly innocuous marks can evoke feelings of worry and curiosity. Known as hypopigmentation, they often hint at something deeper, an underlying message from your body.
White spots can emerge for various reasons: fungal infections that sneak up unnoticed, and the relentless impact of sun damage. White spots on the skin can sometimes be a sign of a condition called vitiligo or pityriasis alba.
For many, these spots are more than skin-deep; they can affect confidence, spark anxiety, and raise questions about health and well-being. A thorough and proper diagnosis needs to be done to get a confirmation of the underlying issues.
But here’s the good news: understanding these spots is the first step toward regaining control and embracing your skin’s journey. In this blog, we’ll explore the common culprits behind white spots, equip you with practical prevention tips, and unveil effective treatment options.
Together, we’ll empower you to take proactive steps toward healthy, glowing, even-toned skin that you can wear with pride.
Because your skin tells a story, it’s time to make sure it’s one of strength, care, and resilience. Let’s dive in! And discuss the types of white spots on the skin.
Read More: Vitiligo Treatment
Read More: Impactguru hospital finder
Table of Contents
- These white dots on my skin—what are they?
- Title: Understanding and Preventing White Patches on the Skin
- What Illness Results In Skin White Spots? What Are The Reasons For White Spots On The Skin?
- Milia
- Prevention
- Vitiligo
- Pityriasis Alba
- Tinea versicolor
- Which Vitamin Deficiency Results In Skin White Spots?
- Conclusion
These white dots on my skin—what are they?
When dead cells or skin proteins get stuck beneath the skin’s surface, white spots may develop. They may also be the consequence of colour loss, or depigmentation, brought on by vitiligo or another illness. Fungal infections, like tinea versicolor, often cause white spots on the skin, especially in humid climates.
Natural remedies, such as aloe vera and turmeric, are often considered for white spots on the skin treatment, but their effectiveness may vary.
Title: Understanding and Preventing White Patches on the Skin
White patches on the skin can occur when skin cells lose their pigment-producing function, often due to conditions like vitiligo, fungal infections, or nutritional deficiencies. These patches are usually more noticeable on darker skin tones and can affect a person’s confidence and appearance.
Skin cells contain melanin, which is responsible for giving skin its color. When these cells are damaged or stop functioning properly, melanin production decreases, leading to the development of pale or white areas on the skin.
To help prevent white patches on the skin, it’s important to maintain healthy skin cells through a balanced diet rich in vitamins B12, D, and minerals like zinc and copper. Proper hygiene, sun protection, and avoiding harsh chemicals or allergens can also support skin health. Infections such as tinea versicolor can lead to white spots, so treating fungal issues promptly is essential.
Regular moisturizing and using sunscreen not only protects skin cells but also helps maintain even skin tone. Early consultation with a dermatologist can help identify the cause and preventthe progression of white patches.
What Illness Results In Skin White Spots? What Are The Reasons For White Spots On The Skin?
White spots on the skin can be caused by the following illnesses or conditions:
- Milia
- Vitiligo
- Pityriasis Alba
- Tinea Versicolor
Let’s dissect these illnesses by learning about their definitions, causes, diagnoses, symptoms & and how to cure white spots on the skin.
Milia
Milia are small, white or yellowish cysts that can appear on the skin, often catching your attention due to their stubborn presence. They form when keratin, a protein found in the skin, hair, and nails, gets trapped beneath the skin’s surface.
These little bumps are commonly found on the face, particularly around the eyes, nose, and cheeks. While they can be bothersome in appearance, the good news is that milia are typically harmless and benign.
Recognizing Milia: The Key Symptoms
Milia might be small, but their presence can be hard to ignore. Here’s what to look for:
- Appearance: These cysts are usually small, dome-shaped, and range from white to yellowish.
- Size: They are typically between 1 to 2 millimetres in diameter—tiny but noticeable!
- Location: Milia often appear around the delicate areas of the face, such as the eyelids, cheeks, and nose, though they can pop up elsewhere on the body.
- Texture: Feel them and you’ll notice they are hard and smooth to the touch.
- Discomfort: Typically painless, milia don’t itch or cause pain, but they can irritate sensitive skin or become uncomfortable if touched too often.
What Causes Milia?
Milia can develop for various reasons, depending on age and skin condition:
- Newborns: In babies, milia are common and usually appear within the first few weeks. These are likely due to the skin’s immaturity.
- Adults and Older Children: For older individuals, several factors can contribute:
- Skin Damage: Blistering, burns, or prolonged sun exposure can lead to milia.
- Heavy Skincare Products: Products that clog pores, such as thick creams or oils, may cause milia to form.
- Skin Conditions: Certain conditions, like epidermolysis bullosa, can make someone more prone to milia.
- Medical Procedures: Procedures like dermabrasion or laser treatments, though effective, can sometimes lead to milia as a side effect.
Diagnosing Milia
Thankfully, diagnosing milia is often straightforward. A healthcare provider can usually identify them just by looking at your skin, as they have a very distinctive appearance. In rare cases, a skin biopsy may be performed to rule out other similar conditions.
How to Treat Milia
The great news is that Milia typically resolves on their own, so you may not need to do anything at all! However, if they persist or cause you distress, there are several treatment options:
- Topical Retinoids: Creams with retinoids can help exfoliate the skin, preventing new milia from forming.
- Chemical Peels: These treatments can help slough off the outer layers of dead skin, reducing the chance of milia buildup.
- Manual Extraction: If the milia don’t go away, a healthcare provider can safely remove them with a sterile needle or blade. This must be done by a professional to avoid infection or scarring.
- Laser Therapy: For persistent milia, laser treatments can be an effective option. Laser therapy has become a popular option in recent years for those seeking advanced white spot on skin treatment solutions.
Prevention
The key to avoiding milia is being mindful of your skincare routine. Future breakouts can be avoided by using non-comedogenic products, or ones that don’t clog pores. Regular follow-ups with a specialist are essential for monitoring the progress of any white spots in a skin treatment regimen.
While milia are usually harmless, it’s always wise to consult a healthcare provider if they become persistent or bothersome.
Vitiligo
Vitiligo is a long-term skin condition that causes patches of skin to lose their natural colour, turning pale white. This occurs when the skin loses melanin, the pigment that gives it its hue. These patches can appear anywhere on the body and may gradually grow in size over time. In some cases, vitiligo can also affect hair and even the inside of the mouth, making it a more widespread condition than just skin deep.
Recognizing Vitiligo: The Key Symptoms
The most noticeable symptom of vitiligo is the appearance of irregular, patchy white spots on the skin, commonly starting on the hands, face, and areas around the body openings or the genitals. Other signs to watch for include:
- Premature greying or whitening of the hair on the scalp, eyebrows, eyelashes, or beard.
- Loss of colour inside the mouth and nose, affecting the mucous membranes.
- Itching and discomfort in the affected areas.
What Causes Vitiligo?
While the exact cause remains unclear, vitiligo is generally considered an autoimmune condition, where the body’s immune system mistakenly targets and destroys the melanocytes—the cells responsible for producing melanin. Several factors may contribute to the onset of vitiligo:
- Genetic predisposition: The risk may be raised by a family history of vitiligo or other autoimmune conditions.
- Environmental triggers: Certain chemicals, stress, or even sunburn can potentially provoke the condition.
- Other autoimmune disorders: People with vitiligo may also have a higher likelihood of developing conditions like thyroid disease, rheumatoid arthritis, or type 1 diabetes.
How is Vitiligo Diagnosed?
Diagnosing vitiligo typically begins with a thorough physical examination and a detailed review of the patient’s medical history. A skin biopsy may also be performed, where a small sample of affected skin is analyzed under a microscope to confirm the diagnosis.
How to Treat Vitiligo?
While there is no cure for vitiligo, several treatment options can help manage the condition and restore the skin’s appearance:
- Topical corticosteroids: These creams or ointments can reduce inflammation and may help restore pigment to the skin.
- Topical calcineurin inhibitors: These medications work to reduce inflammation and are often used when corticosteroids aren’t effective.
- Phototherapy: Exposure to ultraviolet light can stimulate the skin’s melanocytes, promoting repigmentation. Dermatologists usually recommend topical creams or phototherapy as part of a white spots-on-skin treatment plan.
- Depigmentation: In cases where vitiligo is widespread, a depigmenting agent can help lighten unaffected skin to match the white patches.
- Cosmetic options: Makeup, self-tanners, and skin dyes offer a quick way to conceal patches, boosting confidence and self-esteem.
Living with Vitiligo
Though vitiligo presents unique challenges, many people with the condition find ways to embrace their new look and lead fulfilling lives. Treatment can help improve the skin’s appearance, while support from healthcare providers, family, and friends plays a key role in managing the emotional impact.
If you or someone you know is showing symptoms of vitiligo, consulting a healthcare provider can help ensure an accurate diagnosis and a personalized treatment plan.
Pityriasis Alba
Pityriasis Alba is a benign skin condition that may sound complex, but is surprisingly common. It manifests as round or oval patches of pale pink or red skin, often dry and slightly scaly. These patches primarily make an appearance on the face, particularly the cheeks, but they can also show up on the neck, shoulders, and upper arms.
While it might not cause significant discomfort, the aesthetic impact of these patches, especially during sunny seasons, can sometimes affect the confidence of the one suffering.
What Does Pityriasis Alba Look Like?
Symptoms for Pityriasis Alba:
- Colour: Patches start as pink or red and eventually fade into pale, hypopigmented areas.
- Texture: Dry and sometimes scaly.
- Size: Varies between 0.5 to 5 cm.
- Location: Commonly on the face, but also on the neck, shoulders, and arms.
- Itchiness: Rare, but possible.
- Seasonal Fluctuations: Patches are more noticeable in summer (due to tanning of surrounding skin) and less visible in winter.
What Causes Pityriasis Alba?
Causes
While the exact cause remains elusive, certain factors are strongly associated:
- Dry Skin: A key contributor, often seen alongside pityriasis alba.
- Sun Exposure: Makes patches stand out against tanned skin.
- Genetics: A family history of atopic dermatitis or allergic conditions increases the risk.
Interestingly, it is often linked with atopic dermatitis (eczema), though not everyone with pityriasis alba has eczema.
Diagnosis for Pityriasis Alba
Diagnosis is straightforward and involves:
- Visual Inspection: A dermatologist can often confirm it by simply observing the patches.
- Wood’s Lamp Test: Used to highlight hypopigmented areas.
- Skin Scrapings: To rule out fungal infections, ensuring an accurate diagnosis.
Treatment: Managing Pityriasis Alba
Here’s the good news: pityriasis alba is self-limiting and often resolves on its own within a few months to a year. However, managing its appearance and associated dryness can be helpful:
- Hydration Is Key:
- Moisturizing creams restore skin hydration and reduce scaling.
- Reduce Inflammation:
- Mild topical corticosteroids or non-steroidal creams like pimecrolimus can help.
- Sun Protection:
- Regular use of sunscreen prevents tanning, reducing the contrast between patches and surrounding skin.
- Cosmetic Solutions:
- Camouflage creams can temporarily mask the patches for a confidence boost.
Though harmless, pityriasis alba can impact self-esteem, especially in visible areas like the face. Proactively managing dryness, protecting against sun exposure, and seeking medical advice if needed can make a world of difference.
Tinea versicolor
Tinea versicolor, also called pityriasis versicolor, is a surprisingly common yet often misunderstood skin condition caused by an overgrowth of the naturally occurring yeast Malassezia. Normally harmless, this yeast can sometimes grow unchecked, creating visible patches of discoloration on the skin. While not harmful or contagious, the condition can significantly affect confidence and self-esteem. But the good news? It’s treatable, manageable, and preventable!
What Does Tinea Versicolor Look Like?
Symptoms of Tinea versicolor.
If you’ve noticed uneven patches on your skin, you’re not alone. Symptoms often include:
- Discoloured patches: These can be lighter or darker than your natural tone, frequently appearing on the chest, back, neck, or upper arms.
- Mild itching: Some experience mild irritation in the affected areas.
- Scaly texture: These patches may feel rough or flaky.
- Sunlight contrast: A tan may highlight the patches, as they don’t darken like the rest of your skin.
Causes of Tinea versicolor
Blame the yeast—but not entirely. Malassezia lives peacefully on everyone’s skin. However, certain factors can upset the balance:
- Hot and humid climates: Yeast thrives in warm, moist environments.
- Oily skin: Overproduction of oil can create the perfect breeding ground.
- Weakened immunity: A less effective immune system may struggle to keep the yeast in check.
- Hormonal shifts: Fluctuations can spark changes in skin chemistry, encouraging yeast overgrowth.
Diagnosis: Quick and Simple
Your dermatologist can often diagnose tinea versicolor at a glance. For confirmation, a skin scraping or biopsy might be done to detect yeast under a microscope.
Treatment: Getting Your Glow Back
The right treatment can work wonders:
- Topical antifungals: Over-the-counter creams, lotions, or medicated shampoos (with selenium sulfide, ketoconazole, or clotrimazole) target the infection directly.
- Oral antifungals: Severe cases may require oral medications like itraconazole or fluconazole.
- Preventive care: Keeping skin clean, dry, and oil-free is key. Regular use of antifungal
While not life-threatening, tinea versicolor can be emotionally taxing, making you feel self-conscious about your skin. Thankfully, this condition is highly treatable, and with persistence, you can restore your skin’s natural appearance.
Which Vitamin Deficiency Results In Skin White Spots?
White spots on the skin can be caused by deficiencies in several vitamins, including:
Vitamin B12: This powerhouse vitamin keeps your skin vibrant. A deficiency can result in white spots, accompanied by fatigue, weakness, or even tingling sensations.
Vitamin C: Famous for its role in collagen production, a lack of vitamin C could lead to white patches and dull, unhealthy skin.
Vitamin D: The “sunshine vitamin,” as it is sometimes called, is essential for healthy skin and calcium absorption. White dots, which indicate more serious imbalances, could show up if there is not enough.
Folate (Vitamin B9): This vitamin not only supports cell growth but also impacts your skin’s appearance. Low levels can lead to white spots, anaemia, and even digestive troubles.
Conclusion
In conclusion, white spots on the skin, while often harmless, can signal underlying conditions or deficiencies that warrant attention. Understanding their causes—whether it’s fungal infections like tinea versicolor, benign conditions like milia and pityriasis alba, autoimmune disorders like vitiligo, or vitamin deficiencies—is crucial for effective management and prevention.
A proactive approach, including proper diagnosis, tailored treatment, and a focus on skin health, can restore confidence and promote an even-toned complexion. With the right care, these spots can become less of a concern, allowing you to embrace your skin’s unique journey with resilience and pride.
Your skin tells a story, and with knowledge and care, it can be one of health, vitality, and strength.












