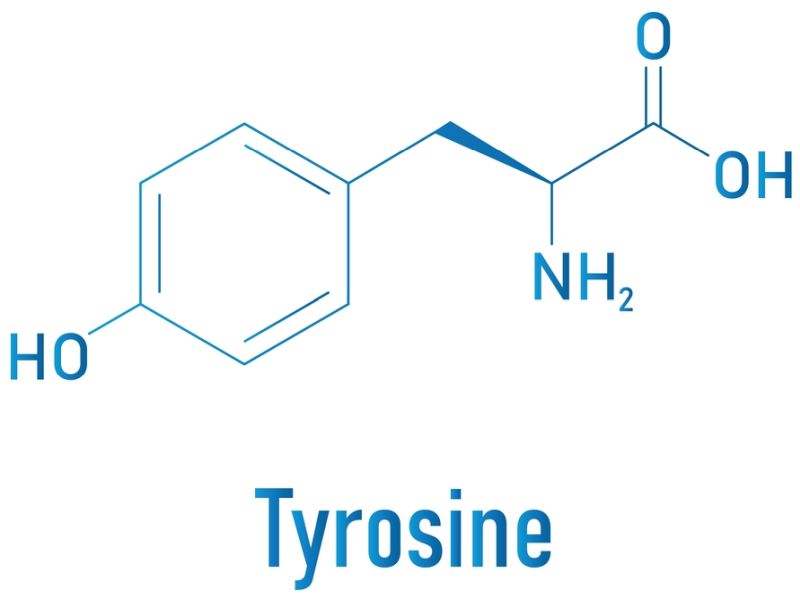
Tyrosinemia is a rare genetic disease distinguished by the body’s inability to crack down the amino acid tyrosine, accumulating toxic byproducts in the blood. Tyrosine is a crucial building block for various proteins in the body, and its proper breakdown is essential for normal metabolic function. There are three main types of tyrosinemia: Type I, Type II, and Type III, each caused by a deficiency in a certain enzyme involved in tyrosine metabolism.
1. Tyrosinemia Type I (HT1): This is the most severe disorder caused by the enzyme fumarylacetoacetate hydrolase (FAH) deficiency. Without this enzyme, toxic byproducts build up, leading to liver and kidney damage. Tyrosinemia Type I usually manifests in infancy and, if left untreated, can be fatal.
2. Tyrosinemia Type II (HT2): Also known as oculocutaneous tyrosinemia or Richner-Hanhart syndrome, a deficiency of the enzyme tyrosine aminotransferase causes this type. It primarily affects the eyes and skin, causing painful skin lesions and eye problems.
3. Tyrosinemia Type III (HT3): This is the rarest form of tyrosinemia, and its exact prevalence is not well-established. It is caused by a deficiency of 4-hydroxyphenylpyruvate dioxygenase (HPD) and can present with neurological symptoms.
Table of Contents
Tyrosinemia Treatment
The treatment for tyrosinemia depends on the type and the extent of organ damage. However, the main goals of treatment are to reduce the levels of tyrosine and its toxic byproducts in the body, to prevent or treat complications, and to improve the quality of life of affected individuals.
The treatment for tyrosinemia varies depending on the type of tyrosinemia a person has, but it may include:
– Dietary management: People with tyrosinemia need to observe a low-protein diet that restricts the consumption of foods that contain tyrosine, such as meats, dairy products, nuts, and beans. They also need to take supplements of vitamins and minerals essential for growth and development. A dietitian can help plan a balanced & nutritious diet that meets the individual needs of every person with tyrosinemia.
– Medication: People with tyrosinemia type I and some cases of type III may benefit from a medication called nitisinone, which blocks the production of toxic substances from tyrosine. Nitisinone can prevent or delay liver failure, kidney damage, rickets, and liver cancer in people with tyrosinemia type I. However, nitisinone also increases the levels of tyrosine in the blood, so it must be used along with a strict low-protein diet. Nitisinone is taken orally once or twice a day for life.
– Liver transplantation: People with tyrosinemia type I who have serious liver damage or liver cancer may need a liver transplant to replace their diseased liver with a healthy one from a donor. A liver transplant can cure tyrosinemia type I, as the new liver can metabolize tyrosine normally. However, a liver transplant is a major surgery that carries risks and requires lifelong immunosuppressive drugs to prevent rejection of the new organ.
– Other treatments: People with tyrosinemia may also need other treatments to address specific complications or symptoms, such as blood transfusions, antibiotics, pain relievers, eye drops, skin creams, or surgery.
What Is Tyrosinemia?
Tyrosinemia is a rare genetic disorder affecting the human body’s ability to break down the amino acid tyrosine, an essential building block of proteins. Tyrosinemia is caused by a deficiency of enzymes involved in the metabolic pathway of tyrosine, leading to the accumulation of toxic byproducts.
Types Of Tyrosinemia

Tyrosinemia Type 1
It is a rare genetic disease affecting how the body breaks down an amino acid called tyrosine. Tyrosine is one of the building blocks of proteins and is found in many foods. Normally, tyrosine is converted into other substances the body uses or eliminated in urine. However, in people with Tyrosinemia Type I, this process is disrupted by a lack of an enzyme called fumarylacetoacetase (FAH). FAH is the last enzyme in a series of steps that break down tyrosine. Without FAH, toxic byproducts of tyrosine metabolism build up in the body and cause damage to various organs, especially the liver and kidneys.
Causes & Risk Factors
Tyrosinemia Type I is caused by mutations in both copies of the FAH gene located on chromosome 15. The FAH gene provides instructions for producing the FAH enzyme. Mutations in the FAH gene can reduce or eliminate the activity of the FAH enzyme, leading to the accumulation of harmful substances like succinylacetone and fumarylacetoacetate. These substances interfere with cellular functions and trigger cell death.
Tyrosinemia Type I is hereditary in an autosomal recessive way, which indicates that both parents must carry a mutated copy of the FAH gene and pass it on to their child. The parents are usually unaffected carriers who do not have symptoms of the disorder. The chance of having a child with Tyrosinemia Type I is 25% for each pregnancy if both parents are carriers.
Tyrosinemia Type I is a rare disorder that affects about 1 in 100,000 newborns worldwide. However, it is more common in certain populations due to genetic factors or environmental influences. For example, Tyrosinemia Type I has a high prevalence of 1 in 1,850 births in the Saguenay-Lac Saint-Jean region of Quebec, Canada, associated with a specific mutation in the FAH gene. This mutation is thought to have originated from a common ancestor who lived in the region several centuries ago.
Clinical Features & Symptoms
The symptoms of Tyrosinemia Type I vary depending on the onset age, the enzyme deficiency’s severity, & the degree of liver and kidney damage. The disorder can be classified into three forms: acute, subacute, and chronic.
The acute form of Tyrosinemia Type I usually appears within the first few months of life and is characterized by severe liver failure, bleeding problems, poor growth, and developmental delay. The liver becomes enlarged and inflamed and may develop cirrhosis or cancer. The kidneys may also be affected by tubular dysfunction, which leads to low levels of phosphate in the blood and causes rickets, which affects bone development. The acute form of Tyrosinemia Type I is often fatal without treatment.
The subacute form of Tyrosinemia Type I typically manifests between 6 & 18 months of age and is characterized by progressive liver disease, kidney problems, rickets, and neurological complications. The liver may show signs of fibrosis or cirrhosis and develop nodules or tumors. The kidneys may have tubular dysfunction or glomerulonephritis, which affects their filtering function. The neurological complications may include seizures, peripheral neuropathy, intellectual disability, or behavioral problems.
The chronic form of Tyrosinemia Type I usually appears after 2 years of age and is characterized by mild to moderate liver disease, kidney problems, rickets, and neurological complications. The liver may have mild fibrosis or cirrhosis but rarely develops cancer. The kidneys may have mild tubular dysfunction or glomerulonephritis. The neurological complications may include learning difficulties, attention deficit hyperactivity disorder (ADHD), or psychiatric disorders.
Some people with Tyrosinemia Type I may not have any symptoms until adulthood, when they may develop liver cancer or kidney failure.
Diagnosis & Screening
Tyrosinemia Type I can be diagnosed by measuring the levels of succinylacetone in blood or urine samples. Succinylacetone is a specific marker for Tyrosinemia Type I that is not found in healthy individuals or other tyrosinemia types. Elevated levels of succinylacetone indicate a deficiency of FAH enzyme activity.
Tyrosinemia Type I can also be diagnosed by genetic testing identifying FAH gene mutations. Genetic testing can confirm the diagnosis in people with positive biochemical tests or clinical symptoms. It can also identify carriers who do not have symptoms but can pass on the mutated gene to their children.
Tyrosinemia Type I can be detected before birth by prenatal testing that analyzes fetal DNA from amniotic fluid or chorionic villus samples. Prenatal testing can be offered to couples who are at risk of having a child with Tyrosinemia Type I, such as those who have a family history of the disorder or belong to a high-risk population.
Tyrosinemia Type I can be detected after birth by newborn screening that analyzes blood samples from heel pricks. Newborn screening can identify babies who have Tyrosinemia Type I before they develop symptoms and start treatment as soon as possible. Newborn screening for Tyrosinemia Type I is available in some countries, like Canada, the United States, and some European countries.
Tyrosinemia Type 2
Tyrosinemia Type II is a rare genetic disorder affecting tyrosine metabolism, an amino acid essential for protein synthesis. Tyrosine is normally broken down by a series of enzymes in the liver and other tissues, but in people with Tyrosinemia Type II, one of these enzymes, called tyrosine aminotransferase (TAT), is deficient or defective. This causes tyrosine to accumulate in the blood and other body fluids, leading to various health problems.
Causes & Genetic Basis
Tyrosinemia Type II is caused by mutations in the TAT gene located on chromosome 16, which encodes the enzyme TAT. The TAT gene mutations can be inherited from one or both parents, who may be carriers of the condition without showing any symptoms. Tyrosinemia Type II follows an autosomal recessive mode of inheritance, meaning that both TAT gene copies must be mutated for the disorder to occur. The chance of having a child with Tyrosinemia Type II is 25% if both parents are carriers, 50% if one parent has the disorder and the other is a carrier, and 100% if both parents have the disorder.
Signs & Symptoms
The main symptoms of Tyrosinemia Type II are related to the accumulation of tyrosine in the eyes, skin, and nervous system. The most common signs are:
– Eye problems: Excessive tearing, redness, pain, sensitivity to light, and inflammation of the cornea (keratitis) result from the deposition of tyrosine crystals in the eye tissues. This can cause vision loss or blindness if left untreated.
– Skin problems: Thickened, painful, and cracked skin lesions (hyperkeratosis) develop on the palms of the hands and soles of the feet due to increased development of keratin, a protein that creates the outer layer of the skin. The skin lesions may also affect other body areas, such as the elbows, knees, and face.
– Mental problems: About half of the people with Tyrosinemia Type II have an intellectual disability or developmental delay due to impaired brain function. The severity of mental problems varies from mild to severe and may include learning difficulties, behavioral issues, speech delay, and seizures.
The symptoms of Tyrosinemia Type II usually appear in early childhood, between 2 and 4 years of age, but they may also occur later in life. The severity & progression of the disorder depends on the type and location of the TAT gene mutation and the amount of dietary tyrosine intake.
Diagnostic Approaches
The diagnosis of Tyrosinemia Type II is based on:
– Blood tests: Elevated levels of tyrosine and its metabolites in the blood indicate a problem with tyrosine metabolism. A normal range for plasma tyrosine is 40 to 90 micromol/L, while people with Tyrosinemia Type II may have levels above 500 micromol/L.
– Genetic tests: Molecular analysis of the TAT gene can confirm the diagnosis & identify the specific mutation causing the disorder. Genetic testing can also be utilized for prenatal detection or carrier screening.
– Skin biopsy: A part of skin tissue can be evaluated under a microscope for signs of hyperkeratosis and tyrosine deposits.
Treatment
The treatment of tyrosinemia type II involves a combination of dietary restriction and medication. The main goal is to lower the amount of tyrosine and its harmful metabolites in the body. This can be achieved by:
– Following a low-protein diet that limits foods rich in tyrosine and phenylalanine, such as meat, dairy, nuts, and beans. Special foods and formulas may be prescribed to ensure adequate nutrition and growth.
– Taking a drug called nitisinone blocks the production of toxic byproducts from tyrosine. Nitisinone can also reduce the need for a strict diet, as it allows some tolerance for tyrosine intake.
– Monitoring blood levels of tyrosine and other amino acids regularly to adjust the diet and medication dosage as needed.
– Treating eye and skin complications with topical or oral medications, surgery, or laser therapy.
Prognosis
The prognosis for people with Tyrosinemia Type II depends on several factors, such as:
– The type and severity of symptoms
– The age at diagnosis and initiation of treatment
– Adherence to dietary restriction and medication
– The presence of other health conditions or complications
With early diagnosis and appropriate treatment, many people with Tyrosinemia Type II can lead normal or near-normal lives. However, some people may experience permanent or progressive damage to the eyes, skin, or brain, affecting their quality of life and life expectancy.
Tyrosinemia Type 3
Tyrosinemia type III is a rare genetic disorder affecting tyrosine metabolism, an amino acid essential for protein synthesis and various biochemical pathways. Tyrosine metabolism involves a series of enzymes that break down tyrosine into simpler molecules that can be used for energy production or other uses. Tyrosinemia type III can result from a deficiency of one of these enzymes, 4-hydroxyphenylpyruvate dioxygenase (4-HDP). This enzyme converts 4-hydroxyphenylpyruvate, a byproduct of tyrosine breakdown, into homogentisic acid, further processed by other enzymes.
The lack of 4-HDP enzyme leads to the accumulation of 4-hydroxyphenylpyruvate and other related compounds in the blood and urine. These compounds can interfere with normal brain function and cause neurological problems. The main symptoms of tyrosinemia type III are intellectual disability, seizures, and intermittent ataxia, which is a loss of balance and coordination that occurs periodically. Unlike other types of tyrosinemia, type III does not affect the liver or cause liver failure.
Tyrosinemia type III is inherited in an autosomal recessive manner that encodes the 4-HDP enzyme and must be mutated for the condition to occur. The HPD gene is located on chromosome 12. The mutations that cause tyrosinemia type III can vary in individuals and families. Some mutations result in a complete absence of 4-HDP enzyme activity, while others reduce its activity to varying degrees.
Tyrosinemia type III is very rare; only a few cases have been reported worldwide. The exact prevalence & incidence of this condition are unknown. It may be more common in certain populations or regions where consanguineous marriages (marriages between relatives) are more frequent.
Diagnosis & Management
The diagnosis of tyrosinemia type III is based on clinical features, biochemical tests, and genetic tests. Clinical features include the presence of intellectual disability, seizures, and intermittent ataxia, as well as the absence of liver problems or other signs of other types of tyrosinemia. Biochemical tests measure the levels of tyrosine and its metabolites in the blood and urine. Elevated levels of 4-hydroxyphenylpyruvate and other compounds indicate a defect in tyrosine metabolism. Genetic tests can confirm the diagnosis by finding mutations in the HPD gene.
The management of tyrosinemia type III involves treating the symptoms and preventing complications. Anticonvulsant medications can help control seizures. Physical therapy & occupational therapy can help improve balance and coordination. Dietary restriction of tyrosine & phenylalanine (another amino acid that can be converted into tyrosine) can help reduce the accumulation of toxic metabolites & improve neurological function. However, the optimal level of dietary restriction is not well established and may vary depending on the severity of the enzyme deficiency and the individual’s response to treatment. A nutritionist can help design a suitable diet plan that meets each patient’s nutritional needs and preferences.
Research & Advances
The research on tyrosinemia type III is limited due to its rarity and lack of animal models. Most studies have focused on describing the clinical features, biochemical abnormalities, and genetic mutations of individual cases or small groups of patients. Some studies have also explored the molecular mechanisms and enzymatic properties of 4-HDP deficiency.
There is no cure for tyrosinemia type III at present, but some potential therapies are being investigated. Gene therapy, which involves introducing a normal copy of the HPD gene into the cells of patients, may offer a way to restore 4-HDP enzyme activity and correct tyrosine metabolism. Enzyme replacement therapy, which involves administering synthetic or recombinant 4-HDP enzymes to patients, may also provide a way to bypass the genetic defect and reduce the accumulation of toxic metabolites. However, these approaches are still in the experimental stages and face many challenges, such as safety, efficacy, delivery, immunogenicity, and cost.
Tyrosinemia type III is a rare and complex disorder that requires multidisciplinary care and follow-up. More research is needed to understand its pathophysiology, natural history, diagnosis, treatment, and outcome.
Tyrosinemia Treatment Cost In India
The only effective treatment for tyrosinemia type 1 is a drug called nitisinone, which blocks the production of harmful substances and prevents further damage to the organs. Nitisinone also reduces the dietary requirement of tyrosine and phenylalanine, another amino acid affected by the disorder. However, nitisinone is a very expensive drug that was not easily available in India until recently. The annual cost of nitisinone treatment for a child with tyrosinemia type 1 ranged from ₹ 2.2 crore to ₹ 6.5 crore, depending on the dosage and weight of the patient. This made it unaffordable for most families and inaccessible for many patients who needed it urgently.
Fortunately, this situation has changed dramatically in the past year, thanks to the efforts of Indian drug companies and government agencies. With the support of the Department of Biotechnology and the Ministry of Science and Technology, four Indian companies have developed and manufactured generic versions of nitisinone at a fraction of the original cost. The new nitisinone capsules are priced at ₹ 2.5 lakh per year, nearly 100 times cheaper than the imported drug. This has made tyrosinemia treatment affordable and accessible for hundreds of patients across India who can now hope for a better quality of life and survival.
Conclusion
In conclusion, understanding tyrosinemia is crucial for early detection and effective management of this rare genetic disorder. The diverse symptoms and types highlight the complexity of the condition, emphasizing the need for a comprehensive approach to diagnosis and treatment. With advancements in medical research and technology, various treatment options are available, offering hope for improved outcomes & a better quality of life for individuals affected by tyrosinemia.
Increased awareness, early intervention, and ongoing research are essential components in the ongoing effort to enhance our understanding and address the challenges associated with this condition. Ultimately, fostering collaboration among healthcare professionals, researchers, and affected individuals is essential to advance knowledge and treatment strategies for tyrosinemia.
Tyrosinemia treatment often involves ongoing medical expenses, including medication, specialized diets, and periodic medical check-ups. Crowdfunding provides a democratic and accessible means for individuals to raise funds, ensuring that financial constraints don’t hinder access to life-saving treatments. Crowdfunding makes expensive healthcare more accessible.












