Tuberculosis (TB) is a highly infectious bacterial disease primarily caused by Mycobacterium tuberculosis, affecting the lungs but can also impact other parts of the body. Tuberculosis causes long-term health challenges, requiring consistent medical treatment and monitoring to prevent its spread. Characterized by symptoms such as persistent cough, fever, night sweats, and weight loss, TB poses significant public health challenges, particularly in low- and middle-income countries. Certain medical conditions, like diabetes, are known to be risk factors for tuberculosis, making individuals more vulnerable to the disease.
Despite being a preventable and treatable disease, TB remains one of the leading causes of morbidity and mortality worldwide, with millions of new cases reported annually. The complexity of TB management is compounded by the emergence of multidrug-resistant strains, necessitating ongoing research, enhanced public health strategies, and global cooperation to combat its spread. Some common risk factors of tuberculosis include living in crowded conditions, poor ventilation, and lack of access to healthcare.
Read More: Tuberculosis Treatment
Table of Contents
What Is Tuberculosis?
The bacteria Mycobacterium tuberculosis is the main cause of tuberculosis (TB), an infectious disease. This pathogen predominantly affects the lungs, leading to pulmonary tuberculosis, but it can also impact other parts of the body, including the kidneys, spine, and brain. TB spreads through the air when an infected person coughs, sneezes, or talks, releasing tiny droplets containing the bacteria that can be inhaled by others.
The disease has been known for centuries, characterized by common tuberculosis symptoms including a persistent cough, fever, and night sweats that can last for weeks. However, many individuals infected with the bacterium may remain asymptomatic, a condition known as latent tuberculosis infection (LTBI), wherein the bacteria are present in the body but inactive, posing no immediate health threat and not being contagious. Early detection of tuberculosis symptoms can lead to more effective treatment and a better outcome.
Due to the complexity of the disease, tuberculosis treatment often requires strict adherence to the prescribed regimen to prevent drug resistance. The global burden of tuberculosis remains significant, particularly in developing countries, where factors such as poverty, overcrowding, and inadequate healthcare systems exacerbate its spread. Socioeconomic determinants, including malnutrition and lack of access to medical care, contribute to higher susceptibility and transmission rates. Additionally, the emergence of drug-resistant strains of TB poses a major challenge to public health efforts, complicating treatment options and requiring more intensive management strategies.
Tuberculosis causes severe damage to the lungs if left untreated, leading to chronic respiratory issues. TB is particularly dangerous for individuals with compromised immune systems, such as those with HIV/AIDS, as it can lead to severe health complications and increased mortality rates. The World Health Organization (WHO) recognizes TB as a public health emergency and emphasizes the importance of global surveillance and preventive measures to control its spread.
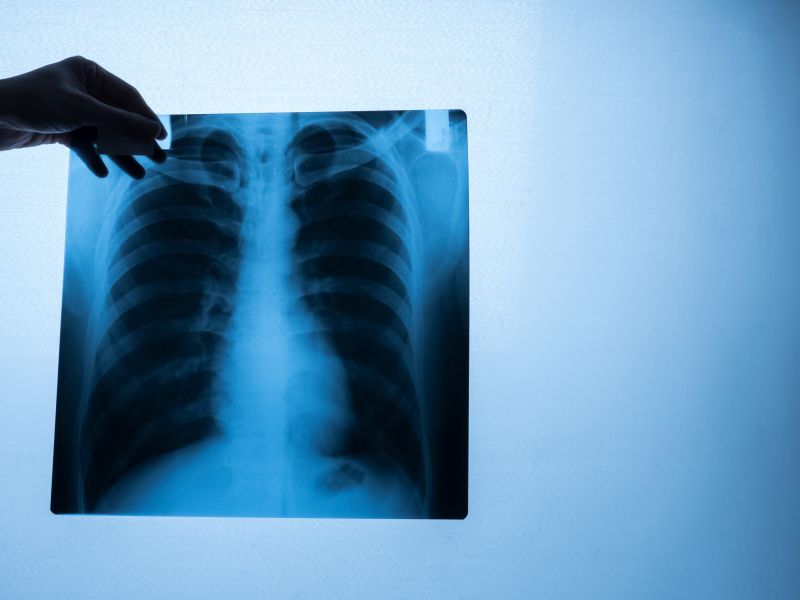
A tuberculosis diagnosis often requires a combination of a skin test, blood test, and chest X-ray to confirm the presence of the infection. Continuous research into TB pathogenesis, vaccine development, and innovative diagnostic methods remains crucial in the fight against this ancient yet persistent disease.
Also Read- Common Communicable Diseases In India: A Detailed Guide
Types Of Tuberculosis
Tuberculosis (TB) can be classified into several types based on various factors, including the site of infection, the presence of symptoms, and the strain of the bacteria. Following are some of the main types of tuberculosis:
- Pulmonary Tuberculosis:
- This is the most common form and occurs when TB bacteria infect the lungs. Symptoms include a persistent cough, chest pain, coughing up blood, and weight loss.
- Extrapulmonary Tuberculosis:
- This occurs when TB spreads outside the lungs to other parts of the body, such as the kidneys, spine, brain, or lymph nodes. Symptoms vary depending on the affected area.
- Latent Tuberculosis:
- The TB germs are still in the body at this point, but they are dormant and not producing any symptoms. Individuals with latent TB are not contagious but can develop active TB later.
- Active Tuberculosis:
- This is when the bacteria are active and multiply, causing symptoms. Active TB can be contagious, especially pulmonary TB.
- Miliary Tuberculosis:
- A rare but severe form of extrapulmonary TB, miliary TB occurs when the bacteria spread through the bloodstream to multiple organs, forming small lesions resembling millet seeds.
- Drug-Resistant Tuberculosis:
- This occurs when the TB bacteria develop resistance to the drugs used to treat it. The two main types are:
- Multi-Drug Resistant TB (MDR-TB): Resistant to at least isoniazid and rifampicin, the two most powerful first-line anti-TB drugs.
- Extensively Drug-Resistant TB (XDR-TB): Resistant to isoniazid, rifampicin, any fluoroquinolone, and at least one of three injectable second-line drugs.
- This occurs when the TB bacteria develop resistance to the drugs used to treat it. The two main types are:
- Tuberculous Meningitis:
- This is a form of extrapulmonary TB that affects the membranes covering the brain and spinal cord, leading to severe complications if not treated promptly.
- Bone and Joint Tuberculosis:
- This type affects the bones and joints, commonly seen in the spine (Pott’s disease). Each type of TB requires different diagnostic and treatment approaches, highlighting the importance of accurate diagnosis and medical intervention.
There are various types of tuberculosis, each affecting different parts of the body or having unique characteristics.
Causes And Risk Factors Associated With Tuberculosis
1. Transmission of Mycobacterium Tuberculosis
- Airborne Infection: TB spreads through the air when a person with active TB in their lungs or throat coughs, sneezes, speaks, or sings, releasing bacteria into the air. Others nearby can then inhale these bacteria.
- Close Contact: Those who live with or spend a lot of time near a person with active TB are more likely to get infected.
2. Weakened Immune System
- HIV/AIDS: People with HIV are at a significantly higher risk of developing TB because their immune systems are compromised.
- Other Health Conditions: Conditions like diabetes, kidney disease, and certain cancers can weaken the immune system, increasing TB susceptibility.
- Age: The very young and the elderly are at higher risk due to weaker or ageing immune systems.
3. Poverty and Living Conditions
- Overcrowding: People in crowded living conditions are at higher risk due to prolonged close contact. Due to its infectious nature, tuberculosis causes widespread concern in densely populated areas.
- Poor Ventilation: Bacteria can linger in the air longer in poorly ventilated spaces, increasing the risk of transmission.
- Malnutrition: Poor nutrition weakens the immune system, making people more susceptible to infections, including TB.
4. Lifestyle Factors
- Smoking: Tobacco use increases the risk of TB infection and worsens TB outcomes.
- Substance Abuse: Alcohol and drug abuse can weaken the immune system and increase the risk of contracting TB.
- Homelessness: People experiencing homelessness are at higher risk due to crowded shelters and limited access to healthcare.
5. Healthcare Access and Delayed Diagnosis
- Limited Healthcare Access: Inadequate access to healthcare can lead to delays in TB diagnosis and treatment, allowing the disease to spread. In some cases, tuberculosis causes an intense immune response, leading to inflammation in the affected tissues.
- Drug Resistance: In cases where TB bacteria are resistant to common antibiotics (MDR-TB and XDR-TB), treatment becomes more difficult, prolonging infectious periods and increasing transmission risks.
6. Migration and Travel
- TB is more common in certain regions, including parts of Asia, Africa, and Eastern Europe. People travelling to or from these regions may be at increased risk, particularly if they come from a low-incidence country with little exposure.
TB can remain latent, meaning the person is infected but doesn’t show symptoms and isn’t contagious. Early diagnosis and consistent tuberculosis treatment are essential for preventing the spread of the infection. However, under conditions like weakened immunity, latent TB can activate, leading to active, contagious TB.
Symptoms Of Tuberculosis
Tuberculosis can be either inactive or active. People with latent TB don’t have symptoms and aren’t contagious, while those with active TB do. Here are the main symptoms of active TB:
1. Persistent Cough
- Lasts longer than 3 weeks.
- May produce phlegm or mucus.
- Coughing up blood is possible in advanced cases.
2. Chest Pain
- Often occurs when coughing or breathing deeply.
3. Fever
- Typically low-grade and may be worse in the evening.
4. Night Sweats
- Severe sweating, often soaking clothes or bed sheets.
5. Fatigue and Weakness
- General feelings of tiredness and a lack of energy.
6. Loss of Appetite and Weight Loss
- Often a gradual reduction in appetite leads to noticeable weight loss.
7. Shortness of Breath
- Particularly if the infection has caused damage to lung tissue.
Extrapulmonary TB Symptoms (if TB spreads outside the lungs)
- Lymph Nodes: Swelling, especially in the neck.
- Bones and Joints: Pain and inflammation.
- Kidneys: Blood in the urine.
- Meningitis: Headache, neck stiffness, and confusion if TB infects the brain or spinal cord.
If someone experiences these symptoms, especially in areas with a high TB prevalence, they should seek medical advice and testing, as early treatment can prevent complications and transmission.
Diagnosis For Tuberculosis
Diagnosing tuberculosis (TB) involves a combination of tests, physical exams, and reviewing medical history to detect an active or latent TB infection. In some cases, tuberculosis symptoms may mimic those of other respiratory infections, making diagnosis challenging. Healthcare providers emphasize the importance of early tuberculosis diagnosis to prevent the spread of this contagious disease. Health professionals monitor patients closely during tuberculosis treatment to check for side effects and ensure effective recovery. Here are the primary methods used:
1. Medical History and Physical Exam
- Symptoms Review: Cough lasting three weeks or more, chest pain, coughing up blood, fever, fatigue, night sweats, and weight loss.
- Risk Factor Assessment: Recent travel to TB-prevalent regions, known exposure, or underlying conditions (e.g., HIV) that may weaken the immune system.
2. Tuberculin Skin Test (TST) / Mantoux Test
- Tuberculin is injected in a very small amount under the skin. After 48-72 hours, the site is checked for a raised bump, which indicates exposure to TB bacteria.
- A positive result doesn’t confirm active TB; it only indicates exposure or a latent infection. Further tests are needed.
3. Interferon-Gamma Release Assays (IGRAs)
- Blood Test (e.g., QuantiFERON-TB Gold or T-SPOT.TB): Measures the immune system’s reaction to TB bacteria.
- Used to confirm latent TB infection, especially in people with previous BCG vaccination.
4. Sputum Tests
- Sputum Smear Microscopy: Checks a sample for acid-fast bacilli (AFB) under a microscope.
- Sputum Culture: A more sensitive test where bacteria are grown in a lab, though it can take weeks.
- Molecular Tests (e.g., Xpert MTB/RIF): Rapid test detecting TB bacteria DNA and resistance to rifampicin, a common TB drug.
5. Chest X-Ray
- Helps to identify lung abnormalities indicative of active TB.
- Often used to differentiate active TB from latent TB infection.
6. CT Scan
- In cases where chest X-rays are inconclusive, CT scans provide a more detailed view of lung abnormalities.
7. Biopsy
- In cases where TB affects organs other than the lungs (extrapulmonary TB), a biopsy of affected tissue can help confirm diagnosis.
The diagnostic approach depends on the type of TB (active or latent), the patient’s symptoms, and their risk profile.
Treatment For Tuberculosis
Tuberculosis treatment typically involves a combination of antibiotics taken over several months to fully eradicate the infection. Identifying the types of tuberculosis is crucial, as it determines the treatment approach and level of contagion.
Here’s an overview of the standard treatment approach:
1. Initial Phase (Intensive Phase)
- Duration: 2 months
- Medications: Four main antibiotics are used:
- Isoniazid
- Rifampicin
- Ethambutol
- Pyrazinamide
- These medications are taken daily to reduce the bacterial load quickly.
2. Continuation Phase
- Duration: Usually 4 months, but maybe longer for certain forms of TB.
- Medications: Only two drugs are continued:
- Isoniazid
- Rifampicin
- The goal is to eliminate the remaining bacteria.
3. Directly Observed Therapy (DOT)
- In some cases, healthcare providers recommend DOT, where a healthcare worker supervises the patient’s medication intake. This ensures adherence to the regimen and helps prevent antibiotic resistance.
4. Multidrug-Resistant TB (MDR-TB) Treatment
- For strains resistant to first-line antibiotics (e.g., Isoniazid and Rifampicin), a longer course (18-24 months) of second-line drugs is used, which may include:
- Fluoroquinolones (e.g., Levofloxacin, Moxifloxacin)
- Injectable agents (e.g., Amikacin, Kanamycin)
- Other options depend on susceptibility testing.
- Newer medications, such as Bedaquiline and Delamanid, may be used in complex cases.
5. Latent TB Infection (LTBI) Treatment
- For individuals with latent TB infection (no symptoms but positive TB test), treatment aims to prevent active TB development:
- Isoniazid (6-9 months)
- Rifampicin (4 months)
- Isoniazid and Rifapentine together (once weekly for 12 weeks)
Important Considerations
- Adherence: Completing the full course is crucial to avoid relapse and resistance.
- Side Effects: Monitor for side effects, especially liver issues, as some TB drugs can be hepatotoxic.
- Regular Monitoring: Liver function tests, vision exams (for Ethambutol), and hearing tests (for injectable drugs) may be required.
Patients undergoing tuberculosis treatment should maintain a balanced diet and healthy lifestyle to support their immune system. Always consult a healthcare provider to ensure the best treatment plan based on individual health, TB strain, and any resistance patterns. A thorough medical evaluation is necessary if someone presents with tuberculosis symptoms to rule out other conditions. Community education is a crucial component of tuberculosis prevention, as it raises awareness about symptoms and encourages people to seek medical help.
Conclusion
In conclusion, tuberculosis remains a significant global health challenge, characterized by its infectious nature and varied presentation. Understanding the causes, symptoms, and treatment options is crucial for effective prevention and management. Despite advancements in medicine, TB continues to pose threats, particularly in vulnerable populations facing socioeconomic hardships and limited access to healthcare. People with weakened immune systems are at higher risk of developing tuberculosis symptoms, which can lead to severe health complications. Public health initiatives, ongoing research, and increased awareness are essential in combating this ancient disease.
By fostering a collaborative global approach and leveraging resources like crowdfunding for treatment access, we can make strides in reducing the burden of tuberculosis and safeguarding health for all. Tuberculosis prevention includes promoting good hygiene practices, such as covering the mouth when coughing and regular handwashing. Staying informed and proactive is key to controlling TB’s spread and ultimately eradicating its impact on communities worldwide.












