Sickle cell anemia is a rare genetic disease that influences the red blood cells, leading to various complications and health challenges for those affected. This hereditary condition is led by a mutation in the HBB gene, responsible for producing hemoglobin—the protein that carries oxygen in the blood. Individuals with sickle cell anemia inherit two abnormal hemoglobin genes, one from each parent, resulting in the creation of abnormal hemoglobin, known as hemoglobin S.
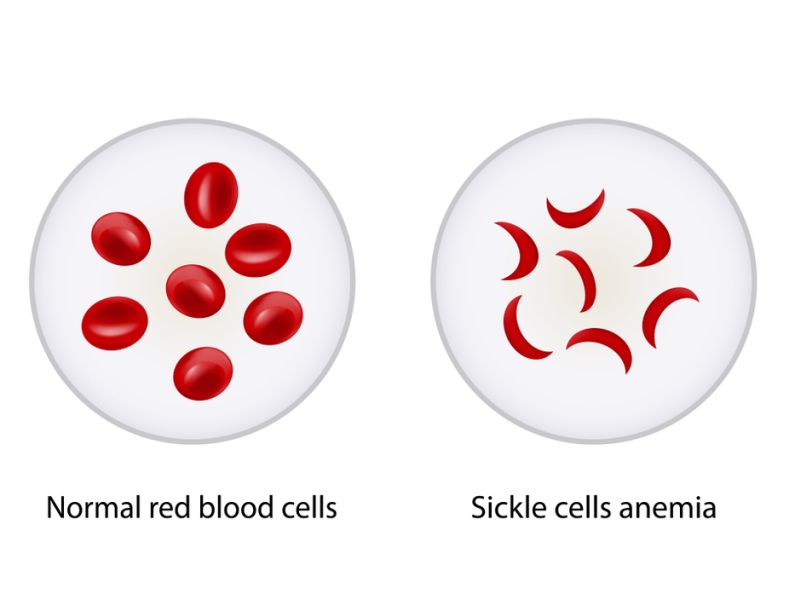
One of the hallmark features of sickle cell anemia is the abnormal shape of red blood cells. Normally, red blood cells are round & flexible, allowing them to move easily through blood vessels. However, in patients with sickle cell anemia, the hemoglobin S causes red blood cells to grow rigid & take on a crescent or sickle shape. These abnormally shaped cells can get fixed in blood vessels, causing blockages that impede the normal flow of blood. This can result in a range of symptoms & complications, including pain, anemia, and organ damage.
Preventive measures, such as newborn screening and genetic counseling, play a crucial role in managing sickle cell anemia. Early detection allows for prompt intervention and supportive care, improving outcomes for individuals with the condition. Despite ongoing research and advancements in treatment options, living with sickle cell anemia remains a lifelong challenge that requires comprehensive care, multidisciplinary support, and a collaborative effort between healthcare providers, patients, & their families.
Table of Contents
- Sickle Cell Anemia Symptoms
- Treatment Available For Sickle Cell Anemia
- Causes Of Sickle Cell Anemia
- Sickle Cell Anemia Definition
- Sickle Cell Anemia Diagnosis
- Sickle Cell Anemia Types
- Difference Between Sickle Cell Anemia And Thalassemia
- Sickle Cell Anemia Treatment Cost In India
- Risk Factors
- Outlook / Prognosis
- Conclusion
Sickle Cell Anemia Symptoms
It’s important to note that the severity of symptoms can vary from person to person, and some individuals may experience milder symptoms while others may have more severe manifestations.
1. Pain Crises:
– Vaso-Occlusive Crises: These are episodes of severe pain that occur when the sickle-shaped red blood cells block blood flow to organs and tissues. The pain can be sudden and intense, affecting bones, joints, and other parts of the body.
– Aplastic Crises: A sudden shortage of red blood cells can result in severe anemia, causing fatigue and weakness.
2. Anemia:
– Reduced number of red blood cells & hemoglobin, leading to fatigue, weakness, and paleness.
3. Jaundice:
– The breakdown of red blood cells can result in the release of bilirubin, causing yellowing of the skin and eyes (jaundice).
4. Swelling of Hands and Feet:
– Sickle cell anemia can cause the hands and feet to swell due to blocked blood flow.
5. Frequent Infections:
– Individuals with sickle cell anemia have an increased risk of infections because the spleen, which helps fight infections, may not function properly due to damage or blockage of blood vessels.
6. Delayed Growth:
– In children, sickle cell anemia may lead to delayed growth and puberty.
7. Vision Problems:
– Blood vessels in the eyes can be blocked, leading to vision problems and even blindness.
8. Organ Damage:
– Over time, repeated episodes of blocked blood flow can cause harm to several organs, including the lungs, heart, kidneys, and spleen.
9. Priapism:
– Men with sickle cell anemia may experience prolonged and painful erections due to blockage of blood vessels in the penis.
10. Stroke:
– Sickle cells can restrict blood vessels in the brain, causing a higher risk of stroke, particularly in children.
Individuals with sickle cell anemia need to receive ongoing medical care to manage symptoms, prevent complications, and improve their overall quality of life. If you suspect you or someone you know has sickle cell anemia, it’s essential to contact a healthcare professional for proper diagnosis & management.
Treatment Available For Sickle Cell Anemia
There is no cure for a rare disease known as sickle cell anemia, but medical treatments can help address the symptoms & complications of the disease. The types of treatment for sickle cell anemia and their costs (INR) in India are:
– Antibiotics: These are used to prevent and treat infections, especially in children with sickle cell anemia. Infections can trigger a pain crisis or damage organs in people with the disease. Antibiotics are generally given orally or intravenously, depending on the severity of the infection. The cost of antibiotics can vary depending on the type and duration of treatment, but it can range from Rs. 100 to Rs. 10,000 per month.
– Painkillers: These are used to relieve pain caused by blocked blood vessels or inflammation in people with sickle cell anemia. Painkillers can be over-the-counter drugs like paracetamol or ibuprofen or prescription drugs like opioids or non-steroidal anti-inflammatory drugs (NSAIDs). The cost of painkillers can vary depending on the type and dosage of medication, but it can range from Rs. 50 to Rs. 5,000 per month.
– Hydroxyurea: This is a drug that can reduce the frequency & severity of pain crises & other complications in individuals with sickle cell anemia. It works by increasing the development of fetal hemoglobin, a type of hemoglobin that does not form sickle-shaped cells. Hydroxyurea is taken orally once a day. The cost of hydroxyurea can vary depending on the dosage and brand of medication, but it can range from Rs. 500 to Rs. 2,000 per month.
– Blood transfusions: These are used to increase the number of normal red blood cells and improve oxygen delivery in people with sickle cell anemia. Blood transfusions can be given regularly to prevent complications like stroke or acute chest syndrome or as needed to treat severe anemia or pain crises. Blood transfusions are given intravenously at a hospital or a blood bank. The cost of blood transfusions can vary depending on the availability and quality of blood, but it can range from Rs. 1,000 to Rs. 10,000 per unit of blood.
– Bone marrow transplant: This is the only potential cure for sickle cell anemia. It involves replacing the bone marrow of a person with sickle cell anemia with healthy bone marrow from a donor who has a matching tissue type. Bone marrow transplants can treat the disease by producing normal red blood cells and hemoglobin. However, it is a risky and complex procedure that requires a compatible donor, intensive chemotherapy and immunosuppression, and lifelong follow-up care. The final price of a bone marrow transplant can differ depending on the type of transplant (allogeneic or autologous), the source of donor cells (peripheral blood stem cells), & the hospital charges, but it can range from Rs. 15 lakhs to Rs. 40 lakhs.
The treatment options for sickle cell anemia depend on several factors, like age, severity of symptoms, availability of resources, and personal preferences. People with sickle cell anemia should consult their doctor regularly to monitor their condition and choose the best treatment plan for them.
Causes Of Sickle Cell Anemia
Here’s a detailed explanation of the causes of sickle cell anemia:
1. Genetic Inheritance:
– Sickle cell anemia is a genetic disorder passed down from parents. To have the condition, a person needs to get two copies of the changed gene, one from each parent.
– The mutated gene responsible for sickle cell anemia is located on chromosome 11 and is specifically called the HBB gene.
2. HBB Gene Mutation:
– The HBB gene mutation involves a single nucleotide substitution in the DNA sequence, leading to the replacement of adenine with thymine at a specific position.
– This mutation results in the creation of abnormal hemoglobin, known as hemoglobin S (HbS), instead of the normal hemoglobin A (HbA).
3. Hemoglobin Polymerization:
– Under certain conditions, such as low oxygen levels or dehydration, the abnormal hemoglobin S molecules tend to polymerize or stick together.
– This causes the red blood cells to become rigid and take on a characteristic sickle shape, which can impede blood flow and cause various complications.
4. Red Blood Cell Destruction:
– The sickle-shaped red blood cells are fragile and prone to premature destruction, leading to a shorter lifespan compared to normal red blood cells.
– This increased rate of red blood cell breakdown contributes to anemia, a common feature of sickle cell disease.
5. Vaso-Occlusive Crises:
– The sickle-shaped red blood cells can block small blood vessels, leading to vaso-occlusive crises. These episodes can result in pain, tissue damage, and organ dysfunction.
– The blockages can also cause inadequate oxygen supply to tissues, leading to further complications.
6. Complications:
– Sickle cell anemia can cause various complications, including stroke, organ damage, infections, and other health issues, due to the effects of abnormal hemoglobin and vaso-occlusive events.
7. Heterozygote Advantage:
– Interestingly, individuals who carry only one copy of the mutated gene (heterozygotes) may have a survival advantage in regions where malaria is prevalent. This phenomenon is known as the heterozygote advantage or the malaria hypothesis.
Sickle Cell Anemia Definition
Sickle cell anemia is a rare genetic disease that influences the shape and function of red blood cells. Red blood cells are normally round & flexible, which permits them to carry oxygen throughout the body. However, in people with sickle cell anemia, a mutation in the gene that develops hemoglobin, the protein that brings oxygen to red blood cells, causes some of them to become sickle-shaped, rigid, and sticky. These abnormal cells can block the blood flow in small vessels, causing pain, infections, organ damage, and anemia.
Sickle cell anemia is an inherited medical condition, meaning that it is passed from parents to children through genes. People who inherit 1 copy of the mutated gene from each parent have sickle cell anemia. Individuals who inherit 1 copy of the mutated gene from 1 parent & a normal gene from the other parent have sickle cell trait. They do not have symptoms of the disease, but they can transfer the mutated gene to their children.
Sickle cell anemia is more familiar in people of African, Arabian, and Indian origin. In India, it is estimated that about 1.5 lakh people have sickle cell anemia, and about 10 crore people have sickle cell trait. The disease is prevalent in states like Maharashtra, Madhya Pradesh, Chhattisgarh, Gujarat, Odisha and Tamil Nadu.
Sickle Cell Anemia Diagnosis
The diagnosis of sickle cell anemia can be done at different stages of life, depending on the availability of screening tests and the presence of symptoms. Here are some ways to diagnose sickle cell anemia:
– Blood test: This test can check for the kind of hemoglobin that causes sickle cell anemia. Hemoglobin is the polypeptide in red blood cells that holds oxygen. People with sickle cell anemia have a form of hemoglobin called hemoglobin S, which makes red blood cells sickle-shaped. A blood test can evaluate the amount of hemoglobin S in the blood and confirm the diagnosis of sickle cell anemia.
– Newborn screening: In some countries, such as the United States, all babies are tested for sickle cell anemia as part of routine newborn screening. This is done by taking a small sample of blood from the baby’s heel and sending it to a laboratory for analysis. Newborn screening can help identify babies with sickle cell anemia early and start treatment to prevent complications.
– Prenatal testing: Sickle cell anemia can also be detected before birth by taking a sample of amniotic fluid or placental tissue from the mother’s womb. This can be done by a procedure called amniocentesis or chorionic villus sampling (CVS). Prenatal testing can help parents who have sickle cell anemia or carry the gene to know if their baby will have the disease and make informed decisions about their pregnancy.
– Ultrasound: A special ultrasound machine can assess the chances of stroke in children with sickle cell anemia. Stroke is a severe intricacy of sickle cell anemia that occurs when blood flow to the brain is blocked by sickle cells. The ultrasound uses sound waves to measure blood flow to the brain and detect any abnormalities. This test can be done in children as young as 2 years old and can help doctors decide if they need regular blood transfusions to prevent stroke.
Sickle Cell Anemia Types
There are several kinds of sickle cell anemia, and the classification is based on the combination of hemoglobin variants inherited from both parents. The two main types are:
1. HbSS (Homozygous Sickle Cell Anemia):
– In HbSS, an individual inherits the HbS variant from both parents (HbSS genotype).
– Both alleles of the HBB gene carry the mutation, resulting in the production of abnormal hemoglobin S.
– This is the most serious form of sickle cell anemia, often associated with more frequent and severe complications.
2. HbSC (Heterozygous Sickle Cell Anemia):
– In HbSC, an individual inherits one HbS variant from one parent and one HbC variant from the other parent (HbSC genotype).
– HbC is another abnormal hemoglobin variant. The combination of HbS and HbC leads to milder symptoms compared to HbSS.
– Individuals with HbSC may experience fewer sickle cell crises and complications.
Apart from these main types, there are other variations based on the combinations of hemoglobin variants. Some of the less common types include:
3. HbSβ Thalassemia:
– In this type, one parent transmits the HbS gene, and the other parent transmits a beta thalassemia gene. Thalassemia is another genetic disorder affecting hemoglobin production.
– The combination results in a milder form of sickle cell disease with symptoms that may vary in severity.
4. HbSD, HbSE, HbSO, etc.:
– These are rare combinations where individuals inherit HbS along with other abnormal hemoglobin variants.
– The severity and symptoms can vary depending on the specific combination of hemoglobin variants.
Difference Between Sickle Cell Anemia And Thalassemia
Sickle cell anemia and thalassemia are both genetic disorders that influence hemoglobin, the protein in red blood cells that carries oxygen. However, they have distinct differences:
1. Genetic Basis:
– Sickle Cell Anemia: It is caused by a mutation in the HBB gene, leading to the production of unnatural hemoglobin known as hemoglobin S (HbS).
– Thalassemia: It is caused by mutations in the genes responsible for producing hemoglobin (HBB gene in beta-thalassemia and HBA genes in alpha-thalassemia). Thalassemia results in reduced production of either alpha or beta globin chains.
2. Hemoglobin Abnormality:
– Sickle Cell Anemia: The abnormal hemoglobin S causes red blood cells to become rigid & take on a characteristic sickle shape, leading to problems like vaso-occlusive crises and reduced oxygen delivery.
– Thalassemia: It results in reduced production of normal hemoglobin, leading to anemia. Depending on the type and severity of thalassemia, there may be a deficiency in either alpha or beta globin chains.
3. Symptoms:
– Sickle Cell Anemia: Symptoms include anemia, pain, increased susceptibility to infections, and organ damage due to vaso-occlusive events.
– Thalassemia: Symptoms include anemia, fatigue, weakness, and, in severe cases, bone deformities and organ damage.
4. Inheritance Pattern:
– Sickle Cell Anemia: It follows an autosomal recessive inheritance pattern, meaning both parents must have a mutated gene for a child to inherit the disorder.
– Thalassemia: It also follows an autosomal recessive pattern, with the severity of symptoms depending on the specific combination of mutated genes inherited.
5. Geographic Distribution:
– Sickle Cell Anemia: It is more dominant in populations with African, Mediterranean, Middle Eastern, and Indian ancestry.
– Thalassemia: Its prevalence is higher in populations from the Mediterranean region, Middle East, Southeast Asia, and Africa.
6. Treatment:
– Sickle Cell Anemia: Treatments focus on managing symptoms and complications. Hydroxyurea, blood transfusions, and bone marrow transplantation may be considered in severe cases.
– Thalassemia: Treatment involves regular blood transfusions, iron chelation therapy to manage iron overload, and, in some cases, bone marrow transplantation.
It’s important to note that while both conditions are genetic blood disorders, they are distinct in their genetic basis, impact on hemoglobin, symptoms, and management. Additionally, individuals carrying one mutated gene for either disorder (carriers) generally do not exhibit significant symptoms but can transfer the mutated gene to their offspring.
Sickle Cell Anemia Treatment Cost In India
The average cost of sickle cell anemia treatment in India depends on the severity of the disorder and the treatment prescribed by the doctor. Depending on the treatment, the cost of sickle cell anemia treatment in India ranges between Rs. 2.6 lakhs to Rs. 17 lakhs. However, this is much lower than the cost of treatment in other countries, such as the US, UK, Canada, or Australia.
Risk Factors
1. Genetic Inheritance: Sickle cell anemia is an inherited genetic disorder caused by the presence of two unusual hemoglobin genes, one from each parent.
2. Ethnicity: The condition is more prevalent in certain ethnic groups, particularly those with African, Mediterranean, Middle Eastern, and Indian ancestry.
3. Family History: Individuals with a family history of sickle cell disease are at a higher risk.
Outlook / Prognosis
The survival rate of SCA for children has dropped dramatically over the last few decades thanks to better screening, diagnosis, and prevention of infections. The mortality rate for children with SCA under the age of 20 was 2.6 percent in 1989, compared to 9.3 percent in 1975. A new pneumonia vaccine introduced in 2000 also reduced the mortality rate for children between the ages of 0 and 3 by 68 percent.
However, SCA is still linked to a shorter life span in adults. The average life expectancy of people with SCA is around 54 years, but this figure may vary depending on the type of SCA, the quality of care, and other factors. The most common causes of death in adults with SCA are acute chest syndrome, stroke, pulmonary hypertension, organ failure, and infection.
People with SCA can improve their outlook by following some health tips, such as:
– Taking their medications as prescribed
– Getting regular blood tests and check-ups
– Drinking plenty of water and avoiding dehydration
– Avoiding extreme temperatures and high altitudes
– Eating a healthy & balanced diet rich in folic acid and calcium
– Exercising moderately and regularly
– Getting enough rest and sleep
– Avoiding smoking, alcohol, and drugs
– Managing stress and seeking emotional support
Conclusion
In summary, Sickle Cell Anemia is a complex genetic disorder with significant health implications. While treatment options have advanced, including the use of hydroxyurea and ongoing research into gene therapy, managing the condition necessitates a multidisciplinary approach. Early detection, education, and addressing healthcare disparities are essential components in improving the quality of life for individuals with Sickle Cell Anemia. As awareness grows and medical interventions evolve, there is hope for an improved quality of life for those affected by this challenging condition.
The high costs associated with its treatment, including medications, hospitalization, and ongoing care, often place a heavy financial burden on affected families. A fundraising platform allows communities to come together to fill this void and ensure that no one is denied medical treatment due to financial constraints.












