Myositis, a term derived from the Greek words “myo,” meaning muscle, and “itis,” denoting inflammation, encompasses a group of rare autoimmune ailments that affect the muscles and surrounding tissues. This complex and often misunderstood condition presents various challenges for both patients & healthcare professionals. In this comprehensive blog, we delve into the depths of myositis, exploring its meaning, symptoms, causes, and the evolving landscape of Myositis treatment options.
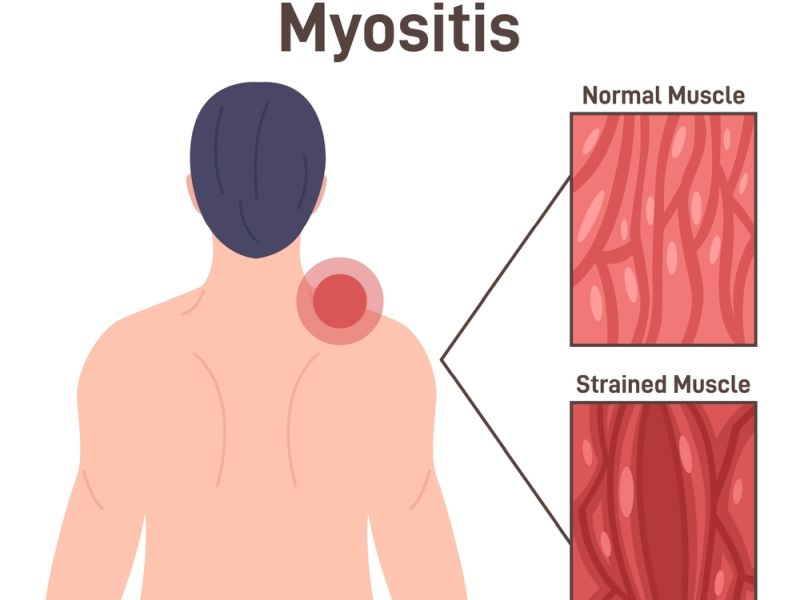
At its core, myositis refers to a category of inflammatory myopathies, conditions characterized by inflammation in the muscles. This inflammation can lead to various degrees of muscle weakness, pain, and fatigue. Myositis is not a singular disorder; rather, it encompasses several subtypes, with dermatomyositis, polymyositis, and inclusion body myositis being the primary classifications. Each subtype exhibits distinct clinical features, making accurate diagnosis and tailored treatment crucial.
Managing myositis requires a multifaceted approach that addresses both the inflammatory component and the associated symptoms. Corticosteroids, immunosuppressive medications, and physical therapy form the cornerstone of treatment, aiming to alleviate inflammation and enhance muscle function. However, the landscape of myositis treatment is evolving, with ongoing research exploring novel therapeutic avenues such as biologic agents and targeted immunomodulatory therapies. As our understanding of myositis deepens, so too does the potential for more effective and personalized treatment strategies.
In conclusion, this exploration into myositis aims to shed light on the intricacies of a condition that often needs more than easy understanding. By comprehensively examining its meaning, symptoms, causes, and the evolving treatment landscape, we hope to contribute to a better-informed dialogue surrounding myositis and empower those affected by this challenging condition.
Table of Contents
Myositis Treatment Options
The treatment of myositis depends on the type, severity, and response of the patient. There is no cure for myositis, but with proper treatment, most patients can manage their symptoms and improve their quality of life. Now, we will discuss some of the treatment options available for myositis patients in India.
Medications
One of the main treatment options for myositis is medication. Medications can help reduce inflammation, suppress the immune system, & prevent further damage to the muscles. Some of the medications used for myositis are:
– Corticosteroids: These are anti-inflammatory drugs that can quickly relieve muscle pain and weakness. They are usually given orally or intravenously. However, they can also cause side effects like weight gain, high blood pressure, diabetes, osteoporosis, & infections. Therefore, they should be used with caution and under close supervision by a doctor.
– Immunosuppressants: These are drugs that lower the activity of the immune system and prevent it from attacking healthy tissue. They are often used in combination with corticosteroids or when corticosteroids are not effective or cause too many side effects. Some examples of immunosuppressants are azathioprine, methotrexate, cyclosporine, mycophenolate mofetil, and tacrolimus.
– Biologic drugs: These are injectable drugs that target specific cells involved in the immune system. They can help modulate the immune response & reduce inflammation. Some examples of biological drugs are rituximab, abatacept, tocilizumab, and anakinra.
– Intravenous immunoglobulin (IVIG): It’s a blood product that includes antibodies from healthy donors. It can help support the immune system and block harmful antibodies that cause muscle damage. It is usually given as an infusion every few weeks or months.
Physical Therapy
Another important treatment option for myositis is physical therapy. It can help improve muscle strength, flexibility, & range of motion. It can also prevent muscle atrophy, contractures, and deformities. Physical therapy may include exercises, stretching, massage, heat or cold therapy, electrical stimulation, ultrasound, and assistive devices.
Physical therapy should be tailored to the individual needs and goals of each patient. It should be done under the guidance of a qualified physical therapist who can monitor the progress & adjust the intensity & frequency of the sessions. Physical therapy should be started as soon as possible after diagnosis and continued throughout the course of the disease.
Lifestyle Changes
In addition to medications and physical therapy, some lifestyle changes can also help manage myositis symptoms and complications. Some of these changes are:
– Having a balanced diet that contains protein, calcium, vitamin D, and antioxidants to support muscle health and prevent bone loss.
– Drinking a good amount of water to stay hydrated & avoid dehydration.
– Avoiding alcohol, tobacco, & other substances that can worsen inflammation or interfere with medications.
– Getting enough rest and sleep to allow the body to heal and recover.
– Managing stress and emotions with relaxation techniques, counseling, support groups, or hobbies.
– Protecting the skin from sun exposure or infections with sunscreen, clothing, moisturizers, and antibiotics.
– Seeking medical attention promptly if any symptoms of infection, fever, rash, breathing difficulty, or chest pain occur.
Myositis Treatment Cost In India
The cost of myositis treatment in India depends on several factors, such as the type and severity of the disease, the duration and frequency of the treatment, the choice of hospital and doctor, the availability of insurance or government schemes, and the exchange rate of the currency. Generally, the cost of myositis treatment in India can range from a few thousand to several lakhs of rupees, depending on the specific treatment plan. The cost of medication is usually the most significant component of myositis treatment costs.
Some of the common medications used for myositis treatment are corticosteroids, immunosuppressants, antimalarials, intravenous immunoglobulin (IVIG), and biologics. These drugs can help reduce inflammation, suppress the immune system, prevent organ damage, and improve muscle strength and function. However, they can also have side effects like weight gain, diabetes, osteoporosis, infections, liver damage, and an increased risk of cancer. Therefore, they need to be prescribed and monitored carefully by a qualified doctor.
The price of myositis medications can vary widely depending on the brand, dosage, frequency, availability, and source. For example, a single dose of IVIG can cost anywhere between Rs 15,000 & Rs 1 lakh, depending on the weight of the patient and the concentration of the product. Similarly, a monthly supply of biologics can cost up to Rs 2 lakhs or more, depending on the type and dosage of the drug. These costs can add up to a substantial amount over time, especially for chronic and progressive forms of myositis, such as the inclusion of body myositis.
In addition to medication, some patients may also require different forms of treatment, like physical therapy, nutritional counseling, psychological counseling, occupational therapy, speech therapy, & supportive devices. These treatments can help improve mobility, function, communication, nutrition, mental health, and quality of life for myositis patients. However, they can also incur additional costs that may not be covered by insurance or government schemes.
One way to reduce the cost of myositis treatment in India is to opt for stem cell therapy, which is an emerging and promising alternative for treating autoimmune diseases. Stem cell therapy involves using the patient’s own stem cells or donor stem cells to repair or replace damaged tissues and organs. Stem cell therapy can potentially offer a permanent cure for myositis by restoring normal immune function and muscle regeneration.
The average cost of stem cell therapy for inclusion body myositis in India is INR 3.2 lakhs ($4,000). The maximum price to be paid for stem cell therapy for IBM in India can go up to INR 4.8 lakhs ($6,000). The cost of myositis treatment in other European countries is approximately $24,000 – $30,000. Therefore, India offers a much more affordable option for stem cell therapy for myositis patients.
However, stem cell therapy is not widely available or approved in India yet. It is still in the experimental stage & requires further research and more clinical trials to establish its safety and efficacy. Therefore, patients who opt for stem cell therapy in India need to be aware of the potential risks and benefits involved. They also need to consult with their doctor & choose a reputable and accredited hospital that offers stem cell therapy for myositis.
Myositis Meaning
Myositis is a set of inflammatory muscle conditions that leads to muscle inflammation and weakness. The term “myositis” is derived from the Greek words “myo,” which means muscle, and “itis,” meaning inflammation. These conditions can affect various muscles in the body and may be associated with other autoimmune diseases.
The exact cause of myositis is often unknown, but it is believed to contain an unusual immune response in which the body’s immunity mistakenly attacks its muscle tissues. Symptoms can include muscle weakness, pain, difficulty swallowing, fatigue, and, in some cases, skin changes.
Types Of Myositis
There are several kinds of myositis, each with distinct characteristics. The main types of myositis include:
1. Dermatomyositis (DM): This type of myositis is characterized by muscle inflammation and skin rash. The rash often appears on the face, eyelids, knuckles, chest, elbows, knees, and back. Dermatomyositis can affect people of any age but is most commonly seen in children and adults between the ages of 40 and 60.
2. Polymyositis (PM): Polymyositis is characterized by muscle inflammation and weakness, but it typically lacks the skin involvement seen in dermatomyositis. Like dermatomyositis, it primarily affects adults, and the exact cause is unknown.
3. Inclusion Body Myositis (IBM): IBM is a progressive muscle disorder characterized by muscle inflammation and weakness. It tends to affect people over the age of 50 and is often considered to be more common in men than in women. IBM is distinct from other forms of myositis, and it is generally resistant to treatment.
4. Necrotizing Autoimmune Myopathy (NAM): NAM is a type of myositis characterized by muscle fiber necrosis (death) and weakness. It can start in isolation or in association with other autoimmune diseases. This type of myositis is often associated with the presence of specific autoantibodies.
5. Juvenile Dermatomyositis (JDM): This form of myositis affects children and is similar to dermatomyositis seen in adults. It involves muscle inflammation and skin rash, and its onset is typically before the age of 18.
6. Overlap Myositis (OM): Some individuals may exhibit features of more than one autoimmune connective tissue disease, such as myositis overlapping with systemic lupus erythematosus or rheumatoid arthritis. This is referred to as overlap myositis.
7. Cancer-Associated Myositis (CAM): In some cases, myositis may be associated with an underlying malignancy, particularly in adults. Cancer-associated myositis involves muscle inflammation and weakness and is often linked to an occult (hidden) cancer.
It’s important to note that myositis can have a considerable effect on an individual’s quality of life, and treatment approaches may involve medications, physical therapy, and other supportive measures. If you suspect you have myositis or are facing symptoms, it’s better to consult with a medical professional for an accurate diagnosis & appropriate management.
Myositis Symptoms
The symptoms can differ depending on the specific type of myositis and the individual. Here are some common symptoms associated with myositis:
1. Muscle Weakness:
– Progressive muscle weakness is a primary symptom of myositis. It typically affects the muscles closest to the trunk of the body, such as those in the hips, thighs, shoulders, and upper arms.
– Difficulty in activities that involve climbing stairs, standing up from a seated position, lifting equipment, or reaching overhead may be noticed.
2. Muscle Pain and Tenderness:
– Individuals with myositis often experience muscle pain and tenderness. This pain can be aching, and it may be more prominent after periods of inactivity or overuse of the affected muscles.
3. Fatigue:
– Persistent fatigue is common in myositis patients. The combination of muscle inflammation and weakness can lead to increased effort and energy expenditure for even simple tasks.
4. Difficulty Swallowing:
– Some forms of myositis, particularly inclusion body myositis, may lead to difficulty in swallowing (dysphagia). This can result in problems with eating and an increased risk of aspiration.
5. Skin Changes:
– Dermatomyositis often involves skin changes, such as a distinctive rash. This rash is typically seen on the face, knuckles, elbows, knees, chest, and back. It may appear as reddish or purplish patches.
6. Joint Pain:
– Joint pain and inflammation may accompany muscle symptoms in some cases, particularly in dermatomyositis.
7. Difficulty Breathing:
– In severe cases or if respiratory muscles are affected, myositis can lead to difficulty breathing. This is more commonly associated with polymyositis.
It’s important to note that the severity & variety of symptoms can differ widely among individuals with myositis.
Myositis Causes
Myositis refers to a group of rare autoimmune diseases that cause inflammation of the muscles. The exact cause of myositis is not well understood, but it is believed to involve a medley of genetic, environmental, and immunological factors. Here are some factors that may contribute to the development of myositis:
1. Autoimmune Response: Myositis is considered an autoimmune ailment, which means that the body’s immune system mistakenly attacks its own tissues. In the case of myositis, the immune system targets the muscles, leading to inflammation. The reasons for this autoimmune response are not fully understood, but it is thought to involve a complex interplay of genetic & environmental factors.
2. Genetic Factors: There may be a genetic predisposition to myositis, as certain genetic markers & variations have been associated with a higher risk of getting the myositis condition. However, having a genetic predisposition does not guarantee that someone will develop myositis.
3. Environmental Triggers: Various environmental factors may trigger or exacerbate myositis in individuals with a genetic predisposition. These triggers can include infections, exposure to certain medications, or other environmental factors. Infections, particularly viral infections, are often implicated as potential triggers for myositis.
4. Medications: Some medications have been linked to the development of myositis. Statins, which are generally used to reduce cholesterol, are known to be associated with a higher risk of myositis in some individuals. Other medications, such as certain antiviral drugs and some antihypertensive medications, have also been linked to myositis in some cases.
5. Environmental Factors: Exposure to several environmental factors, like ultraviolet (UV) radiation from the sun, may contribute to the development or exacerbation of myositis in susceptible individuals.
6. Other Autoimmune Diseases: Myositis is sometimes associated with other autoimmune ailments, like rheumatoid arthritis, lupus, and scleroderma. The presence of one autoimmune disease may increase the risk of developing another.
It’s important to note that myositis is a complex and relatively rare group of diseases, and individual cases can vary widely. Diagnosis and treatment typically involve a multidisciplinary approach, including rheumatologists and other healthcare professionals.
Risk Factors Of Myositis
While the exact cause of myositis is often unknown, various risk factors may increase the likelihood of developing this medical condition. It’s vital to remember that having one or more risk factors does not guarantee that anyone will get myositis. The interaction of various factors likely contributes to the development of the disease. Some of the known risk factors for myositis include:
1. Age and Gender:
– Dermatomyositis and polymyositis often affect individuals between the ages of 30 and 60.
– Dermatomyositis is more common in women than in men.
2. Genetics:
– There is evidence to suggest a genetic predisposition to myositis. Certain genetic factors may increase the susceptibility of an individual to develop the condition.
3. Environmental Factors:
– Exposure to certain environmental factors or triggers may contribute to the development or exacerbation of myositis. These triggers may include infections, toxins, or medications.
4. Infections:
– Viral infections, like HIV, coxsackievirus, and others, have been associated with the development of myositis in some cases.
5. Medications:
– Some medications, such as statins, can trigger myositis in some individuals. However, it’s important to note that not everyone who takes these medications will develop myositis.
6. Autoimmune Diseases:
– Myositis is considered an autoimmune disease, and patients with autoimmune ailments, like lupus or rheumatoid arthritis, may have an increased risk of developing myositis.
7. Cancer:
– In some cases, myositis may be associated with a higher risk of certain cancers, especially in adults with dermatomyositis.
8. Smoking:
– Smoking has been suggested as a potential environmental factor that may increase the chances of developing myositis.
Myositis Diagnosis
To diagnose myositis, a doctor will ask about the symptoms, medical history, and family history of the patient. They will also conduct a medical examination to look for muscle weakness, tenderness, and rash. Some tests that may help confirm the diagnosis are:
– Blood tests to measure the levels of muscle enzymes, like creatine kinase (CK) and aldolase, and antibodies, such as antinuclear antibody (ANA) and anti-Jo-1 antibody
– Muscle biopsy to take a small sample of muscle tissue and examine it under a microscope for signs of inflammation and damage
– Electromyography (EMG) to estimate the electrical activity of the muscles
– Magnetic resonance imaging (MRI) to produce detailed images of the muscles
Myositis Life Expectancy
In general, the prognosis for myositis varies by the form and presence of other conditions, such as interstitial lung disease or autoantibodies. For sporadic inclusion body myositis (sIBM), the life expectancy is usually the same as for those without the disease. For other forms, the life expectancy may be longer or shorter depending on the complications and treatments.
As per The Myositis Association, more than 95 percent of those with dermatomyositis, polymyositis, and necrotizing myopathy are still living more than 5 years after diagnosis. Many might experience only one period of acute illness in their lifetime; others struggle with symptoms for years. Some people may need assistance with daily activities or mobility devices due to muscle weakness.
Lifestyle factors, like smoking, diet, exercise, and stress management, can also influence the life expectancy of someone with myositis. These factors can affect the immune system, inflammation, and muscle function. Therefore, it is important to follow the advice of your doctor and adopt healthy habits that can improve your quality of life.
Is Myositis Curable?
There is no cure for myositis, but medical treatment can help reduce inflammation, prevent muscle damage, improve strength, and relieve symptoms.
Conclusion
In conclusion, myositis is a complex and rare set of autoimmune diseases that affect the muscles, leading to inflammation and weakness. Recognizing the symptoms, which may include muscle pain, weakness, and fatigue, is crucial for early diagnosis and effective treatment. While the exact cause of myositis is not fully known, a combination of genetic & environmental factors is believed to contribute to its development.
As research continues to uncover more about the underlying mechanisms of myositis, advancements in treatment strategies offer hope for better outcomes and enhanced patient care. Myositis treatment involves a spectrum of medical interventions, from medication and therapy to surgical procedures. The cumulative costs can be overwhelming, making crowdfunding an effective solution to provide financial relief.
Crowdfunding taps into the power of community support. Friends, family, and even strangers can come together to contribute, fostering a sense of unity and compassion.












