Myeloproliferative neoplasms (MPNs) include a group of rare but potentially serious blood disorders characterised by the unusual proliferation of blood cells in the bone marrow. These conditions originate in the body’s hematopoietic stem cells, leading to the overproduction of one or more types of blood cells. While MPNs are considered chronic diseases, they can progress over time and may increase the risk of complications like blood clots, bleeding, & even transformation into acute leukaemia.
In recent years, medical advancements in understanding the molecular mechanisms underlying MPNs have led to the development of targeted therapies that mainly target abnormal signalling pathways involved in disease progression. Clinical trials evaluating novel therapeutic agents and treatment strategies are ongoing, offering hope for improved outcomes and quality of life for patients with MPNs. However, managing MPNs remains a complex and evolving field, requiring a multidisciplinary approach involving haematologists, oncologists, & other medical professionals to tailor treatment plans to individual patient needs and optimise long-term outcomes.
Read More: Impactguru hospital finder
Table of Contents
Myeloproliferative Neoplasm Meaning
Let’s break down “myeloproliferative neoplasm” into simpler terms.
1. Myelo-: This part of the word refers to the bone marrow, the porous tissue inside your bones that makes blood cells.
2. Proliferative: This means that something is growing or increasing in number. So, “proliferative” means an abnormal increase in the production of certain types of blood cells.
3. Neoplasm: This is a term for the unusual growth of cells, which can lead to tumour formation.
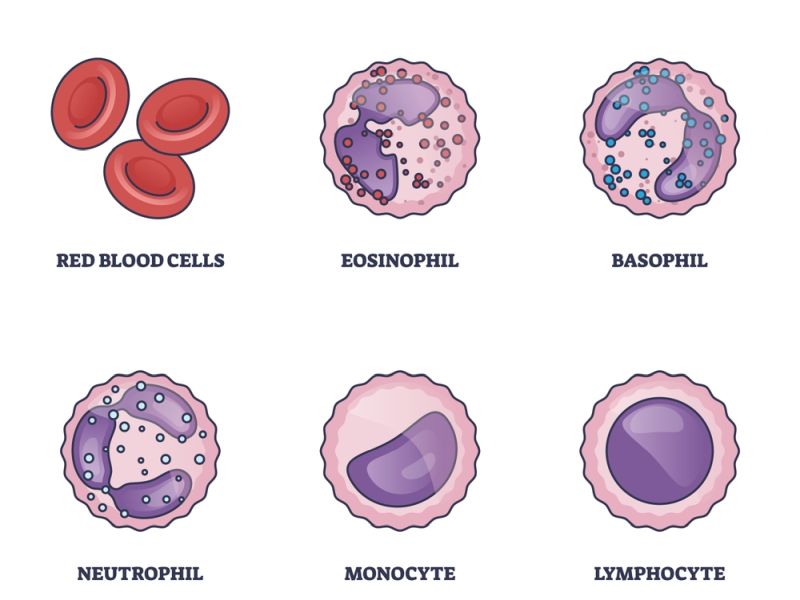
In summary, the myeloproliferative neoplasm is a condition in which the production of certain types of blood cells in the bone marrow increases abnormally, leading to tumours. These conditions can affect different kinds of blood cells, like red, white blood cells, or platelets.
Myeloproliferative Neoplasms Types
There are several types of MPNs, each with its own distinct characteristics and clinical features:
1. Chronic Myeloid Leukemia (CML):
– CML is a type of cancer caused by translocation between chromosomes 9 & 22, known as the Philadelphia chromosome. This translocation causes the formation of the BCR-ABL fusion gene, an oncogene that drives the uncontrolled proliferation of myeloid cells.
– CML typically presents with more mature granulocytes (neutrophils, eosinophils, and basophils) in the blood and bone marrow. It progresses slowly through three phases: chronic, accelerated, and blast crisis.
2. Polycythemia Vera (PV):
– PV is a condition where there is an excessive production of red blood cells, causing increased blood volume and thickness. This can result in signs & symptoms like headache, dizziness, & blurred vision, as well as a higher risk of thrombotic events like stroke or heart attack.
– PV may also be associated with an increase in white blood cells and platelets. It is often caused by a mutation in the JAK2 gene, particularly the JAK2 V617F mutation.
3. Essential Thrombocythemia (ET):
– ET is characterised by the overproduction of platelets (thrombocytosis) in the bone marrow, leading to an increased risk of abnormal blood clotting (thrombosis) or bleeding. However, some patients may be asymptomatic and diagnosed incidentally through routine blood tests.
– Like PV, ET is often associated with mutations in the JAK2 gene, though other mutations, such as CALR or MPL mutations, may also be present.
4. Primary Myelofibrosis (PMF):
– PMF is characterised by the abnormal proliferation of megakaryocytes (precursors of platelets) in the bone marrow, leading to the formation of fibrous tissue & subsequent bone marrow failure. This fibrosis disrupts normal blood cell production, leading to cytopenias (low blood cell counts).
– PMF often presents with symptoms such as anaemia, fatigue, enlarged spleen (splenomegaly), and abdominal discomfort. It can also predispose individuals to thrombotic events or transformation to acute leukaemia.
– Mutations in JAK2, CALR, and MPL genes are frequently observed in PMF, though around 10-15% of cases may be triple-negative (lacking mutations in these genes).
Symptoms Of Myeloproliferative Neoplasms
The symptoms can differ based on the particular type of MPN and the individual, but some common symptoms include:
1. Fatigue: Feeling tired or weak is a common symptom of MPNs, often due to the increased demands on the body from the overproduction of blood cells.
2. Enlarged Spleen: The spleen may enlarge (splenomegaly) due to the excessive accumulation of blood cells. This can cause discomfort in the left upper abdomen.
3. Easy Bruising and Bleeding: MPNs can affect the normal functioning of platelets, which are liable for blood clotting. This can lead to easy bruising, nosebleeds, or prolonged bleeding from minor cuts or injuries.
4. Night Sweats: Some individuals with MPNs may experience night sweats, which can disrupt sleep and lead to feelings of discomfort.
5. Bone Pain: Pain in the bones, particularly in the back, ribs, or legs, may occur due to the overproduction of blood cells in the bone marrow.
6. Itching (Pruritus): Pruritus, or itching, is a common symptom in MPNs, particularly in polycythemia vera (PV). The exact cause of itching in MPNs is not fully known but is believed to be related to increased histamine levels.
7. Headaches: Headaches can occur due to the increased viscosity of the blood in some MPNs, particularly in PV. Increased blood viscosity can also increase the risk of blood clots.
8. Gout: Gout is a kind of arthritis that occurs in individuals with MPNs who have high levels of uric acid due to increased cell turnover, resulting in the buildup of uric acid crystals in the joints.
9. Abdominal Discomfort: Some individuals with MPNs may experience abdominal discomfort or early satiety (feeling full after eating only a small amount) due to an enlarged spleen pressing on the stomach or other abdominal organs.
10. Weight Loss: Unexplained weight loss may occur in some individuals with MPNs, mainly if the condition is advanced or if there are complications such as excessive sweating or loss of appetite.
It’s important to note that not everyone with an MPN will experience all of these symptoms, & some individuals may have additional symptoms not listed here. Additionally, symptoms can vary in severity and may come and go over time. If you are experiencing any of these symptoms, especially if they are persistent or severe, it’s essential to see a medical professional for evaluation & diagnosis.
Myeloproliferative Neoplasms Diagnosis
Diagnosing MPNs can be complex, as symptoms often resemble those of other illnesses. However, a series of tests can help healthcare providers determine the presence of MPNs and the specific type. They are
1. Complete Blood Count (CBC): This is often the first test done. It measures the levels of red cells, white cells, and platelets in the blood.
2. Peripheral Blood Smear: A blood sample is examined under a microscope to determine blood cells’ shape, size, and maturity.
3. Comprehensive Metabolic Panel (CMP): This test includes measurements of blood sugar, electrolyte and fluid balance, kidney function, and liver function.
4. Serum Erythropoietin (EPO) Level: Erythropoietin (EPO) is a hormone that boosts the growth of red blood cells in the body. Abnormal levels can be a sign of MPNs.
5. Serum Iron Studies: These tests measure the amount of iron in the blood & can help distinguish between different types of MPNs.
6. Genetic Testing: Certain genetic mutations are associated with MPNs. Tests can identify mutations such as JAK2, CALR, and MPL.
7. Bone Marrow Biopsy: A small sample of bone marrow is taken and examined for abnormalities in blood cell production.
8. Bone Marrow Aspiration: This procedure involves taking a liquid sample from the bone marrow to look for abnormal cells.
9. Cytogenetic Analysis: This test looks for changes in the chromosomes of cells from the bone marrow.
10. Molecular Testing: This can detect specific gene mutations associated with MPNs.
11. Ultrasound: An abdominal ultrasound can check for an enlarged spleen, which can appear in MPNs.
12. Chest X-ray: This may be done to check for signs of infection or other conditions.
These tests provide a comprehensive view of an individual’s blood and bone marrow health, helping to confirm a diagnosis of MPNs and guide treatment decisions. Remember, only a healthcare provider can diagnose MPNs and recommend the appropriate tests based on individual symptoms and medical history. If you suspect you have symptoms of MPNs, seek medical advice for diagnosis and personalised care.
Myeloproliferative Neoplasms Life Expectancy
Survival rates & life expectancy for patients with MPNs depend on various factors, such as the type of MPN, age, overall health, and stage of diagnosis. Treatments have evolved over the years, and medical care advancements have improved many patients’ outlook.
Polycythemia Vera (PV) is a more common MPN associated with an overproduction of red blood cells. The 5-year survival rate for PV patients is approximately 85%, close to the expected survival of age- and gender-matched healthy individuals. However, at 25 years post-diagnosis, the expected survival drops to around 20%, compared to 55% for healthy, matched individuals.
Essential Thrombocythemia (ET) is another MPN where the bone marrow produces too many platelets. It is considered one of the slowest progressing forms of MPN. Patients with ET have a median overall survival of 18 years, which is relatively favourable compared to other MPNs.
Primary Myelofibrosis (PMF) is the rarest and most aggressive type of MPN. It not only involves an increased production of blood cells but also leads to scarring in the bone marrow, influencing its ability to produce healthy cells. The 5-year survival rate for PMF is around 55%, and at 25 years, the survival rate drops significantly to approximately 10%.
Chronic Myeloid Leukemia (CML), another MPN, has seen remarkable progress in treatment options. More than 70% of men and 75% of women with CML live at least five years following their diagnosis. With the introduction of targeted therapies like imatinib, about 90% of people with CML treated with this medication were alive five years later.
It’s important to note that these statistics are based on large groups of patients and may not necessarily predict individual outcomes. Each patient’s journey with MPN is unique, and survival rates are just one part of the story. Ongoing research and clinical trials continue to seek better treatments and, ultimately, a cure for these complex diseases.
Myeloproliferative Neoplasms Treatment
In India, the treatment of MPNs involves a variety of strategies, each with its own set of costs. Understanding these costs is vital for patients & their families navigating their treatment options. The cost of MPN treatment in India varies depending on the type of MPN, the stage of the disease, the specific treatment plan, and the healthcare provider. Here’s a breakdown of some common treatments and their associated costs:
1. Hydroxyurea: As a first-line treatment for conditions like polycythemia vera and essential thrombocythemia, hydroxyurea is relatively affordable, with monthly costs ranging from approximately ₹1,000 to ₹3,000.
2. Interferon Alfa: Used for its anti-proliferative effects on bone marrow, interferon alfa can cost between ₹15,000 to ₹25,000 monthly, based on the dosage and frequency of administration.
3. Ruxolitinib (JAK2 Inhibitor): This targeted therapy is used for myelofibrosis and can be quite expensive, with monthly costs potentially exceeding ₹1,00,000. However, patient assistance programs may help reduce this burden.
4. Anagrelide: Used to lower platelet counts in essential thrombocythemia, anagrelide’s monthly cost can range from ₹4,000 to ₹12,000, depending on the dosage.
5. Stem Cell Transplantation: This is a potential curative treatment for some MPN patients, especially younger individuals with a suitable donor. The price can vary widely but typically ranges from ₹10,00,000 to ₹30,00,000, covering the procedure, hospital stay, and post-transplant care.
It’s important to note that these costs are approximate & can vary based on individual circumstances. Additionally, indirect costs such as travel, accommodation for outstation patients, and loss of income can add to the financial burden.
Conclusion
In conclusion, myeloproliferative neoplasms represent a group of blood disorders characterised by the overproduction of abnormal blood cells. While there are different types of MPNs, they share common symptoms such as fatigue, weakness, and an enlarged spleen. Early detection & management are crucial in improving outcomes for individuals affected by MPNs. With ongoing research & advancements in treatment options, there is hope for better management and quality of life for those living with these conditions.
It’s vital for patients to work closely with their healthcare providers to develop personalised treatment plans tailored to their specific needs. By raising awareness and understanding of MPNs, we can empower people to take control of their health & confidently navigate their journey.
Treatment for MPNs often involves medications, regular check-ups, and sometimes more advanced procedures like stem cell transplants. These expenses can quickly accumulate, making it difficult for individuals and families to afford them. A fundraising website allows them to reach out to a broader network of supporters who can contribute financially to cover these costs.












