As India’s vibrant tapestry of culture and heritage continues to thrive, so does its unwavering spirit in times of adversity. However, amidst the numerous health challenges that the country faces, one particular concern has been rising in recent times, casting a shadow on the healthcare landscape – Mucormycosis, commonly known as “black fungus.” In this blog, we delve into the critical topic of Mucormycosis treatment cost in India, shedding light on the impact of this infection, the number of cases, and the alarming mortality rate that grips the nation.
Mucormycosis, also known as black fungus, is a rare but severe infection caused by a group of fungi called mucormycetes. These fungi are commonly found in soil, fallen leaves, compost, animal dung, and air and can infect the lung, sinuses, brain, and eyes of humans. Mucormycosis is not contagious but mainly affects anyone with a weakened immune system or underlying medical conditions, such as diabetes, cancer, HIV/AIDS, or COVID-19.
Mucormycosis has gained significant attention in India as a secondary complication affecting individuals recovering from COVID-19 or those with weakened immune systems. With its sudden surge, this deadly fungal infection has become a formidable adversary, posing serious challenges to the country’s healthcare system. As the number of cases rises, it becomes essential for the community to understand the treatment options available and the financial implications that come with them.
Mucormycosis has become a significant health concern in India, especially after the second wave of the COVID-19 pandemic. According to the World Health Organization (WHO), the prevalence of mucormycosis in India is expected to be 140 per million population, which is over 80 times higher than the prevalence in other developed countries. The overall mucormycosis prevalence in India is 0.14 cases per 1000 population, ranging between 208 177 and 137 807 cases. The mean of attributable deaths per year is 65 500 (38.2%).
The surge of COVID-19 associated mucormycosis cases in India has been linked to several factors, such as poor glycaemic control in diabetic patients, excessive use of steroids and other immunosuppressive drugs in treating severe COVID-19 cases, lack of infection prevention & control measures in health care facilities, and shortage of antifungal drugs and diagnostic tests. The most common type of mucormycosis reported in India is rhino-orbital cerebral mucormycosis, which affects the nose, eyes, and brain. This type of mucormycosis has a high % mortality rate of 50% and often requires surgical removal of the infected tissue or organ to save the patient’s life.
The Government of India has taken several steps to address the mucormycosis crisis in the country. These include making mucormycosis a notifiable disease under the Epidemic Diseases Act 1897; allocating additional vials of antifungal drugs to states; waiving import duty on antifungal drugs; issuing guidelines on prevention, diagnosis, and management of mucormycosis; and setting up special wards and helplines for mucormycosis patients. However, more efforts are needed to improve awareness, diagnosis, and treatment of this deadly infection among healthcare workers and the general public.
Whether you’re a patient seeking treatment, a concerned family member, or a compassionate citizen willing to help, this blog will equip you with the knowledge to make a difference. Let us join hands as a united community, driving the necessary changes to combat Mucormycosis and alleviate its impact on the lives of fellow Indians.
Table of Contents
Mucormycosis Treatment Cost In India

The treatment cost of mucormycosis in India varies depending on the severity of the infection, the type of antifungal drug used, the duration of treatment, and the availability of health insurance. The average cost of treating a mucormycosis patient in India can vary from Rs 3 lakh to Rs 10 lakh (US$ 4,000 to US$ 13,500), excluding the surgery cost. The cost can be higher for patients who need prolonged hospitalization or multiple surgeries. The cost can also vary depending on the state and the hospital where the patient is treated.
One of the main challenges in treating mucormycosis is the high cost of the antifungal drugs and surgeries required. The standard treatment for mucormycosis involves intravenous administration of liposomal amphotericin B (L-AmB), a potent antifungal agent that can kill the fungus & prevent its spread. However, L-AmB is expensive and scarce in India. Each vial of L-AmB costs around INR 7,000, and a patient may need up to 100 vials for a complete course of treatment. This means that the total cost of L-AmB alone can range from INR 7 lakhs to INR 13 lakhs per patient.
In addition to L-AmB, patients may also need other drugs, such as posaconazole and isavuconazole, which are also costly and not easily available. Moreover, patients may require multiple surgeries to remove the infected tissues and organs, such as the eye, nose, jaw, or brain. These surgeries can add to the financial burden of the patients and their families.
Fortunately, there are ways to reduce the mucormycosis treatment cost in India. One way is to use the conventional form of amphotericin B (C-AmB), which is much cheaper than L-AmB. C-AmB costs around INR 350 per vial and has a similar efficacy as L-AmB in treating mucormycosis. However, C-AmB has more side effects than L-AmB, especially on the kidneys. Therefore, C-AmB should be used with caution and under close monitoring of blood creatinine levels. Blood creatinine is a waste product that reflects kidney function. If blood creatinine levels are high, the kidneys are damaged, and C-AmB should be stopped or reduced.
Another way to lower the mucormycosis treatment cost in India is to avail of government schemes and insurance policies that cover the expenses of the disease. For instance, Maharashtra has announced that it will provide free treatment for mucormycosis patients under its Mahatma Jyotiba Phule Jan Arogya Yojana (MJPJAY) scheme. Similarly, other states like Gujarat, Rajasthan, Tamil Nadu, Kerala, and Delhi have also announced free or subsidized treatment for mucormycosis patients under their respective health schemes.
Moreover, some private hospitals and NGOs have also come forward to help mucormycosis patients with affordable treatment options. For example, Ayu Health is a network of hospitals that offers quality care for mucormycosis patients at a reasonable price. Ayu Health provides L-AmB at INR 3,500 per vial and posaconazole at INR 1,500 per tablet. It also provides free consultations with ENT specialists and surgeons for mucormycosis patients.
Mucormycosis is a serious disease that requires timely diagnosis and treatment to prevent fatal outcomes. However, the high cost of treatment can deter many patients from seeking medical help or completing their course of therapy. Therefore, raising awareness about the disease and its treatment options among the public and healthcare providers is vital. It is also essential to ensure adequate supply and distribution of antifungal drugs and surgical equipment nationwide. Moreover, it is necessary to provide financial support and assistance to mucormycosis patients and their families through government schemes and private initiatives.
Read More: Impactguru hospital finder
Factors Affecting The Mucormycosis Treatment Cost In India
The recent surge of mucormycosis cases in India has raised concerns regarding the treatment cost and its impact on patients’ financial well-being. Several factors contribute to the overall expense associated with mucormycosis treatment in India.
Medical Interventions
The type of medical intervention required for treating mucormycosis can significantly impact the overall treatment cost. This includes antifungal medication administration, oxygen therapy, blood transfusions, and other supportive care measures aimed at stabilizing patients’ health.
Diagnostic Procedures
Diagnostic tests such as CT scans, MRI scans, tissue biopsies, and histopathological examinations are essential for accurate diagnosis and monitoring of mucormycosis. The expenses associated with these diagnostic procedures contribute to the overall treatment costs.
Medication Expenses
Antifungal drugs form a crucial part of mucormycosis treatment. However, some antifungal medications may be expensive or not readily available in some areas of India. The accessibility and affordability of these medications directly influence the total treatment expenditure.
Hospitalization Costs
Mucormycosis often requires hospitalization for an extended period due to its severe nature. The duration of hospital stay contributes significantly to the overall cost burden on patients since it involves charges related to bed occupancy, nursing care services, laboratory investigations, administrative fees, etc.
Surgical Interventions
Invasive surgical interventions like debridement or amputation may be necessary depending on the severity and extent of fungal infection spread within a patient’s body. Such surgeries involve additional costs, including operating room charges, anesthesia fees, surgeon’s fees, post-operative recovery expenses, etc., further increasing the overall treatment expenditure.
Post-Treatment Care
After successful completion of primary treatments (medication courses or surgeries), follow-up visits, consultations with doctors, specialists, physiotherapy sessions, rehabilitation programs, etc., may be required. The costs associated with post-treatment care contribute to the overall treatment expenses for mucormycosis patients in India.
Various factors, including medical interventions, diagnostic procedures, medication expenses, hospitalization costs, surgical interventions, and post-treatment care, influence mucormycosis treatment costs in India. Understanding these key factors can help healthcare providers develop strategies to optimize treatment outcomes while minimizing patient financial burdens.
What Is Mucormycosis?
Mucormycosis, also known as black fungus, is a rare but serious fungal infection that can affect different body parts. It is caused by a group of molds called mucormycetes, commonly found in soil, decaying organic matter, and animal dung. These molds can enter the body through inhalation, ingestion, or skin contact and cause various types of infections depending on the site of entry and the person’s underlying health condition.
Mucormycosis is a severe infection that requires immediate medical attention. If left untreated or not diagnosed early, it can spread rapidly and cause severe complications, including tissue death (necrosis), organ failure, and even death. The infection is diagnosed through a combination of clinical evaluation, imaging tests (such as CT scans or MRIs), and laboratory analysis of tissue or fluid samples. Early detection is crucial for effective treatment.
Types And Symptoms Of Mucormycosis
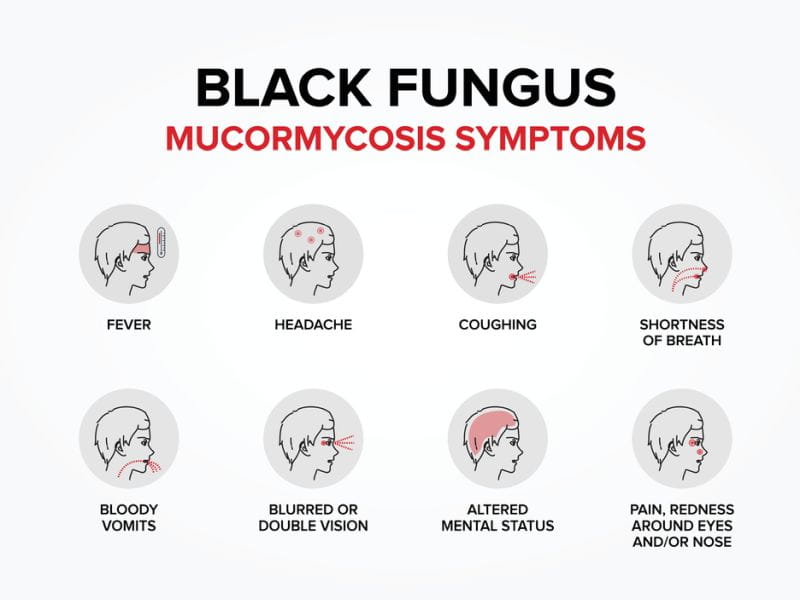
Mucormycosis can be classified into five main types based on the organ or tissue involved:
1) Rhino-orbital-cerebral mucormycosis:
- This is the most common type of mucormycosis, which affects the nose, sinuses, eyes, and brain. It usually occurs in people with diabetes, especially diabetic ketoacidosis, or who have had a transplant or surgery involving the nose or sinuses. The symptoms may include:
– Runny nose or nasal congestion
– Black or bloody discharge from the nose
– Facial pain or swelling
– Headache or fever
– Blurred or double vision
– Bulging or displacement of the eye (proptosis)
– Loss of vision or blindness
– Tissue death (necrosis) of the affected area
2) Pulmonary mucormycosis:
- This type affects the lungs and respiratory tract and can cause pneumonia. It usually occurs in people with a weakened immune system due to cancer, chemotherapy, organ transplant, HIV/AIDS, or long-term use of steroids or immunosuppressants. The symptoms may include:
– Cough or chest pain
– Shortness of breath or difficulty breathing
– Fever or night sweats
– Coughing up blood (hemoptysis)
– Weight loss or fatigue
3) Cutaneous mucormycosis:
- This type affects the skin and soft tissues, especially around a break in the skin, such as a wound, burn, or injection site. It can also occur after a bite from an animal or insect that carries the fungus. The symptoms may include:
– Redness, swelling, or pain at the affected site
– Blisters, ulcers, or black scabs on the skin
– Fever or chills
– Drainage of fluid from the wound
4) Gastrointestinal mucormycosis:
- This type affects the stomach and intestines and can cause ulcers, bleeding, perforation, or obstruction. It usually occurs in infants and young children who have malnutrition, prematurity, or low birth weight. It can also occur in adults with inflammatory bowel disease, cancer, or HIV/AIDS. The symptoms may include:
– Abdominal pain or cramps
– Nausea or vomiting
– Diarrhea or constipation
– Blood in the stool (hematochezia) or vomit (hematemesis)
– Weight loss or dehydration
5) Disseminated mucormycosis:
- This is the most severe type of mucormycosis, which occurs when the infection spreads from one site to other organs such as the spleen, heart, brain, and kidneys. It can be life-threatening &requires immediate treatment. It usually occurs in people who have a very low white blood cell count (neutropenia) due to cancer, chemotherapy, bone marrow transplant, or other conditions. The symptoms may include:
– Fever or shock
– Altered mental status or confusion
– Seizures or coma
– Organ failure/multiple organ dysfunction syndrome (MODS)
Mucormycosis Treatments In India

Mucormycosis is treated with a combination of antifungal medications and surgery. The treatment depends on the type & seriousness of the viral infection, the patient’s overall health condition, and the response to therapy. The main goals of treatment are:
– To stop the growth and spread of the fungus
– To remove any dead or infected tissue
– To restore normal function & appearance of the affected area
– To prevent complications and recurrence
The antifungal medication for mucormycosis is liposomal amphotericin B, which is given intravenously at a dose of 5 mg/kg per day (or 10 mg/kg per day for brain involvement). Liposomal amphotericin B is a potent drug that can kill the fungus effectively, but it can also cause side effects such as kidney damage, electrolyte imbalance, or infusion reactions. Therefore, it needs to be monitored closely and adjusted according to the patient’s condition.
Other antifungal medications used for mucormycosis are posaconazole or isavuconazole, which are given orally. These drugs are less toxic than amphotericin B, but they may not be as effective or available in some settings. They can also interact with other medications that the patient may be taking.
The duration of antifungal therapy for mucormycosis varies depending on the type and extent of the infection, but it usually lasts for several weeks to months. Once the infection is stabilized and improved, the patient may be switched to a lower dose or a different drug for maintenance therapy.
Surgery is an essential part of mucormycosis treatment, as it helps to remove any necrotic (dead) or infected tissue that may be blocking vital structures or harboring the fungus. Surgery also helps to reduce the fungal load and improve the delivery and penetration of antifungal drugs. Surgery may involve procedures such as:
– Debridement or excision of the affected tissue or organ
– Endoscopic or open sinus surgery to clear the nasal passages and sinuses
– Orbital exenteration or evisceration to remove the eye and surrounding structures
– Craniotomy or skull base surgery to access the brain and cranial nerves
– Thoracotomy or lung resection to remove part of the lung
– Laparotomy or bowel resection to remove part of the intestine
– Skin grafting or reconstructive surgery to repair the skin defects
Surgery for mucormycosis may be challenging and risky, as it may involve delicate and vital structures already damaged by the infection. Therefore, it requires a multidisciplinary team of experts, such as ENT surgeons, neurosurgeons, ophthalmologists, plastic surgeons, thoracic surgeons, gastroenterologists, and infectious disease specialists. Surgery should be done as early as possible, but only after adequate antifungal therapy has been initiated.
Prevention Of Mucormycosis

Mucormycosis is a preventable disease, especially in the context of COVID-19. Some of the preventive measures that can be taken are:
– Controlling diabetes and blood sugar levels
– Avoiding or limiting the use of steroids and other immunosuppressive drugs
– Following appropriate infection prevention and control practices in healthcare settings
– Wearing masks and gloves when handling soil, compost, or animal dung
– Cleaning and disinfecting any wounds or injuries promptly
– Seeking medical attention for any persistent or unusual symptoms
Mucormycosis is a severe fungal disease that can influence anyone with a weakened immune system. It can cause severe complications and death if not treated early and aggressively. Therefore, it is crucial to know mucormycosis’s signs and symptoms and seek medical help immediately. With timely diagnosis and treatment, mucormycosis can be cured and overcome.
Conclusion
In conclusion, the blog explored the critical issue of Mucormycosis, commonly known as “black fungus,” and its treatment cost in India. Mucormycosis is a rare & severe fungal infection that usually affects individuals with weakened immune systems or underlying health conditions, and it has been a matter of growing concern in the country. The blog highlighted the importance of early detection, prompt medical intervention, and the challenges of managing the disease.
The treatment of Mucormycosis in India involves a multidisciplinary approach, requiring collaboration between infectious disease specialists, ENT surgeons, ophthalmologists, and other medical professionals. The primary treatment for Mucormycosis is aggressive antifungal therapy, typically involving intravenous administration of drugs like Amphotericin B, which is often expensive and can have adverse side effects. In some medical cases, surgical intervention may be necessary to remove the infected tissue & prevent the spread of the fungus.
The blog emphasized the significant impact of the 2021-2022 COVID-19 pandemic in India, as many Mucormycosis cases emerged as post-COVID complications. The surge in demand for antifungal drugs, coupled with supply chain disruptions, contributed to an escalation in treatment costs, making it a significant concern for patients and healthcare providers alike.
It also highlighted the potential financial burden on patients and their families due to the high cost of Mucormycosis treatment in India. Accessing timely and effective treatment becomes an additional challenge for individuals who need adequate health insurance or financial means. This underscores the urgent need for government intervention and policy measures to address the accessibility and affordability of essential medicines for rare diseases like Mucormycosis.
Furthermore, the blog acknowledged the importance of public awareness campaigns and education on Mucormycosis, its risk factors, symptoms, and preventive measures. Timely diagnosis can significantly improve treatment outcomes and reduce the economic burden on patients and the healthcare system. The Indian healthcare system must form a comprehensive strategy to combat the rise of Mucormycosis cases, including increasing the availability and affordability of antifungal medications, enhancing medical infrastructure and capacity to handle the disease, and strengthening infection control measures in hospitals.
In conclusion, Mucormycosis is a severe and complex medical challenge in India, requiring concerted efforts from all stakeholders – the government, healthcare professionals, pharmaceutical companies, and society as a whole. By fostering collaboration, raising awareness, and prioritizing affordability and accessibility of treatment, India can effectively combat Mucormycosis and mitigate its impact on public health. Ultimately, the goal should be to ensure that every affected individual receives timely and affordable treatment, leading to improved treatment outcomes and a better quality of life for the patients.
Mucormycosis treatment can be prohibitively expensive, especially for vulnerable communities with limited financial resources. By pooling small contributions from a global network of donors, a crowdfunding website empowers everyone to make a meaningful impact, enabling patients to access critical medical care without worrying about financial burdens.












