Langerhans Cell Histiocytosis (LCH) is a rare ailment distinguished by the abnormal accumulation and proliferation of Langerhans cells, which are a kind of immune cell. This medical condition can influence individuals of all ages, but it primarily occurs in children between the ages of 1 and 15. While the exact cause of LCH remains unknown, it is believed to involve a dysregulation of the immune system, leading to the accumulation of these abnormal cells in various organs and tissues throughout the body.
Explore different types, symptoms, treatment options, and more. Whether you’re a patient, caregiver, or curious learner, we aim to provide valuable information to help you navigate the complexities of LCH. Early detection & prompt treatment initiation are vital for achieving the best possible outcomes and minimizing long-term complications associated with LCH.
Table of Contents
- Langerhans Cell Histiocytosis Treatment
- What Is Langerhans Cell Histiocytosis?
- Langerhans Cell Histiocytosis Types
- Symptoms Of Langerhans Cell Histiocytosis
- Causes Of Langerhans Cell Histiocytosis
- Risk Factors & Complications Of Langerhans Cell Histiocytosis
- Diagnosis & Tests For Langerhans Cell Histiocytosis
- Conclusion
Langerhans Cell Histiocytosis Treatment
The treatment for LCH depends on the type and stage of the disease, as well as the age and general health of the patient. There are different types of treatment available for LCH in India, such as:
– Chemotherapy: This is the use of drugs to destroy or stop the development of cancer tumors. Chemotherapy is often given through injections or pills. Chemotherapy can be used alone or in a mixture with other treatments, such as steroids or targeted therapies. Chemotherapy is usually given for 6 to 12 months, depending on the response and side effects. The cost of chemotherapy for LCH in India ranges from INR 50,000 to INR 2,00,000 per cycle, depending on the drugs used and the hospital chosen.
Steroid therapy: This is the use of drugs that lessen inflammation & suppress the immune system. Steroids can help shrink the tumors or lesions caused by LCH and relieve some symptoms, such as pain, swelling, or fever. They can be given orally or intravenously and are often used along with chemotherapy or other treatments. The cost of steroid therapy for LCH in India ranges from INR 5,000 to INR 20,000 per month, depending on the dose and duration.
– Targeted therapies: These drugs target specific molecules in cancer cells’ growth or survival. Targeted therapies can help block or interfere with these signals and stop the cancer cells from spreading or growing. It can be given orally or intravenously. Targeted therapies are usually used for patients who have high-risk LCH or who do not respond to chemotherapy or other treatments. The cost of targeted therapies for LCH in India ranges from INR 1,00,000 to INR 5,00,000 per month, depending on the drug and the hospital chosen.
– Radiation therapy: This therapy utilizes high-energy beams to destroy cancer cells or shrink tumors. It can be given externally or internally. It can be used for patients who have localized LCH that does not respond to other treatments or who have serious symptoms that influence their quality of life. This therapy can also prevent bone fractures or nerve damage caused by LCH lesions. The cost of radiation therapy for LCH in India ranges from INR 50,000 to INR 1,50,000 per session, depending on the type and dose of radiation and the hospital chosen.
– Surgery: This is the removal of tumors or lesions by an operation. Surgery can be used for patients who have isolated LCH that affects only one bone or organ and who do not have any signs of systemic disease. Surgery can also remove LCH lesions that cause complications, such as bleeding, infection, or obstruction. The cost of surgery for LCH in India ranges from INR 1,00,000 to INR 10,00,000, depending on the type and extent of surgery and the hospital chosen.
– Stem cell transplant: This medical procedure involves replacing unhealthy bone marrow with donor stem cells, which are immature blood cells capable of developing into various types of blood cells. Stem cell transplant can be used for patients who have high-risk LCH that does not respond to additional treatments or who have relapsed after initial treatment. Stem cell transplant can also be used for patients who have severe damage to their bone marrow caused by LCH or its treatment. The cost of stem cell transplant for LCH in India ranges from INR 10,00,000 to INR 30,00,000, depending on the type and source of stem cells and the hospital chosen.
The choice of treatment for LCH depends on many factors, such as the patient’s age and condition, the type and stage of the disease, the availability & affordability of the treatment options, and the preferences and expectations of the patient and their family. The treatment plan should be discussed with a team of experts who specialize in treating LCH and can provide comprehensive care and support throughout the treatment process.
What Is Langerhans Cell Histiocytosis?
Langerhans cell histiocytosis, or LCH, is a rare disorder that occurs when abnormal cells called Langerhans cells proliferate and accumulate in different organs of the body. Langerhans cells are a kind of white blood cell that normally help the immune system fight infections. However, in LCH, these cells become clonal and overactive, causing damage to the tissues they infiltrate.
LCH can affect any organ but most commonly involves the skin, bones, lymph nodes, lungs, liver, spleen, bone marrow, or brain. The symptoms & severity of LCH depend on which organs are affected and how many lesions are present. LCH can occur at any age but is more common in children younger than 15.
Langerhans Cell Histiocytosis Types
LCH is classified into three types based on the extent of organ involvement:
– Unifocal LCH: This type affects only one organ or site, usually a bone or the skin. It is also called eosinophilic granuloma. It is the most common and benign form of LCH and often resolves spontaneously or with local treatment such as surgery or radiation.
Multifocal unisystem LCH: This type affects multiple sites within the same organ system, such as various bones or numerous skin lesions. It is also called Hand-Schüller-Christian disease or cutaneous single-system LCH. It is more aggressive than unifocal LCH and may require systemic treatment, such as chemotherapy or steroids.
Multifocal multisystem LCH: This type affects multiple organs or systems, such as the lungs, liver, spleen, bone marrow, or brain. It is also called Letterer-Siwe disease or disseminated LCH. It is the most severe and life-threatening form of LCH and requires intensive systemic treatment, such as chemotherapy or immunotherapy.
Symptoms Of Langerhans Cell Histiocytosis
LCH can affect people of any age, but it is most commonly diagnosed in children between the ages of 1 and 3 years old. The symptoms of LCH can vary widely depending on which parts of the body are affected. Here’s a detailed breakdown of the symptoms:
1. Bone Symptoms:
– Bone pain: Pain in the affected bones is one of the most common symptoms of LCH. The pain may be dull or sharp & can worsen with activity.
– Swelling: Swelling or a lump may develop in the affected bones.
– Fractures: LCH can weaken the bones, making them more prone to fractures. Fractures may occur with minimal trauma.
– Limited mobility: In some cases, LCH can affect joints, causing stiffness and limited range of motion.
2. Skin Symptoms:
– Rash: A rash may appear as red or brown scaly patches on the skin. The rash may be itchy or painful.
– Sores: Open sores or ulcers may develop on the skin, particularly in areas where the rash is present.
3. Organ Involvement:
– Liver: LCH can affect the liver, leading to hepatomegaly (liver enlargement) and jaundice (yellowing of the skin and eyes).
– Spleen: Enlargement of the spleen (splenomegaly) may occur in some cases.
– Lungs: Lung involvement can lead to coughing, shortness of breath, and respiratory distress.
4. Central Nervous System (CNS) Symptoms:
– Headaches: LCH can cause headaches, which may be persistent and severe.
– Neurological symptoms: Based on the place of the lesions in the CNS, neurological symptoms such as weakness, coordination difficulties, and seizures may occur.
5. Endocrine Symptoms:
– Diabetes insipidus: This condition, characterized by excessive thirst and urination, can occur due to LCH affecting the pituitary gland.
– Growth failure: LCH can interfere with the function of the pituitary gland, causing growth hormone insufficiency and growth failure in children.
6. Lymph Node Involvement:
– Enlarged lymph nodes: LCH can cause the lymph nodes to swell, particularly in the neck, armpits, and groin.
7. Eye Symptoms:
– Vision problems: LCH can affect the eyes, leading to symptoms such as blurry vision, redness, and eye pain.
It’s important to note that not all individuals with LCH will experience all of these symptoms, & the severity of signs & symptoms can differ widely from person to person. Additionally, some individuals may have no symptoms at all and may only be diagnosed incidentally through imaging studies or biopsies performed for other reasons.
Causes Of Langerhans Cell Histiocytosis
While the exact cause of LCH remains unclear, several hypotheses have been proposed:
1. Immune Dysregulation: It is believed that LCH may result from dysregulation of the immune system, leading to abnormal proliferation and activation of Langerhans cells. Various factors may trigger this dysregulation, including infections, environmental toxins, or genetic predisposition.
2. Genetic Factors: There is evidence suggesting a genetic component to LCH, as it can sometimes occur in families. However, specific genetic mutations associated with LCH have not been consistently identified. Further research is needed to understand better the genetic factors contributing to the development of LCH.
3. Environmental Triggers: Exposure to certain environmental toxins or infectious agents has been proposed as potential triggers for LCH. However, no specific environmental factor has been definitively linked to the development of the condition.
4. Abnormal Cell Signaling: Dysregulated signaling pathways within Langerhans cells are vital in the pathogenesis of LCH. For example, mutations affecting signaling pathways, such as the mitogen-activated protein kinase (MAPK) pathway, have been implicated in some cases of LCH.
5. Immune Suppression: Some cases of LCH have been reported in individuals with compromised immune systems, such as those receiving immunosuppressive therapy or with underlying conditions that weaken the immune response. This suggests that immune suppression may contribute to the development of LCH in certain individuals.
Overall, Langerhans Cell Histiocytosis is likely a multifactorial disorder with a complex interplay of genetic, immunologic, and environmental factors contributing to its pathogenesis.
Risk Factors & Complications Of Langerhans Cell Histiocytosis
The causes of LCH are not well understood, but some possible risk factors include the following:
– Being born to a parent who has been exposed to specific chemicals like benzene.
– Having a parent who has encountered metal, granite, or wood dust in the workplace.
– A family history of cancer, including LCH.
– Having experienced infections as a newborn.
– Having a personal or familial history of thyroid disease.
– Smoking, especially among young adults.
LCH can cause damage to tissues and organs all over the body if it is not treated. Some of the possible complications include the following:
– Pituitary gland problems, such as diabetes insipidus, which affects the balance of fluids in the body.
– Growth problems, such as short stature or delayed puberty.
– Lung problems, such as pulmonary histiocytosis, which causes breathing difficulties and lung scarring.
– Bone problems, such as osteoporosis, fractures, or deformities.
– Skin problems, such as rashes, ulcers, or hair loss.
– Neurological problems, such as seizures, headaches, or LCH-associated neurodegeneration, which affects the brain and nervous system.
– Endocrine problems, such as hypothyroidism, adrenal insufficiency, or hypogonadism.
– Liver problems, such as hepatitis, cirrhosis, or portal hypertension.
– Spleen problems, such as splenomegaly or hypersplenism.
– Blood problems, such as anemia, thrombocytopenia, or leukopenia.
Diagnosis & Tests For Langerhans Cell Histiocytosis
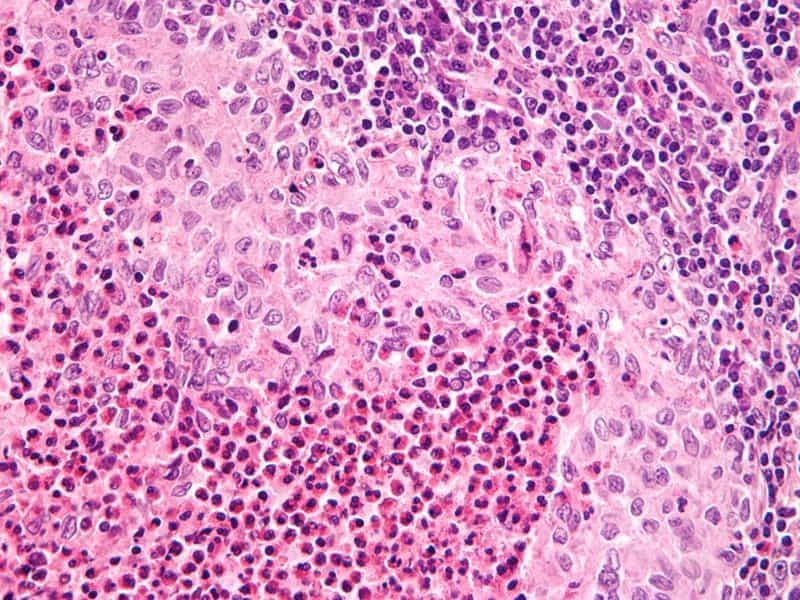
To diagnose LCH, doctors usually perform a biopsy of the affected tissue and examine it under a microscope. They look for CD1a and CD207 proteins, markers of Langerhans cells. They may also do blood tests, imaging tests (such as X-rays, CT scans, MRI scans, or PET scans), and genetic tests to check for mutations in the BRAF or MEK genes involved in the growth and survival of Langerhans cells. Radiology is vital in identifying and monitoring LCH lesions, which can appear as nodules, cysts, or lytic defects in imaging studies.
Conclusion
In conclusion, Langerhans Cell Histiocytosis (LCH) is a rare disorder characterized by the overproduction of Langerhans cells, which can affect various organs & systems in the body. The symptoms of LCH can vary widely depending on the organs involved, ranging from bone pain and swelling to skin rashes and respiratory problems. Diagnosis often consists of a combination of imaging studies, biopsy, and histopathological examination of affected tissues. Collaborative efforts between healthcare providers, researchers, and patients are essential for improving our understanding of LCH and developing more effective treatments in the future.
LCH treatment can be financially crippling, especially in countries like India, where healthcare costs can be prohibitive. Crowdfunding provides a platform for individuals to reach out to a broad audience for financial support.












