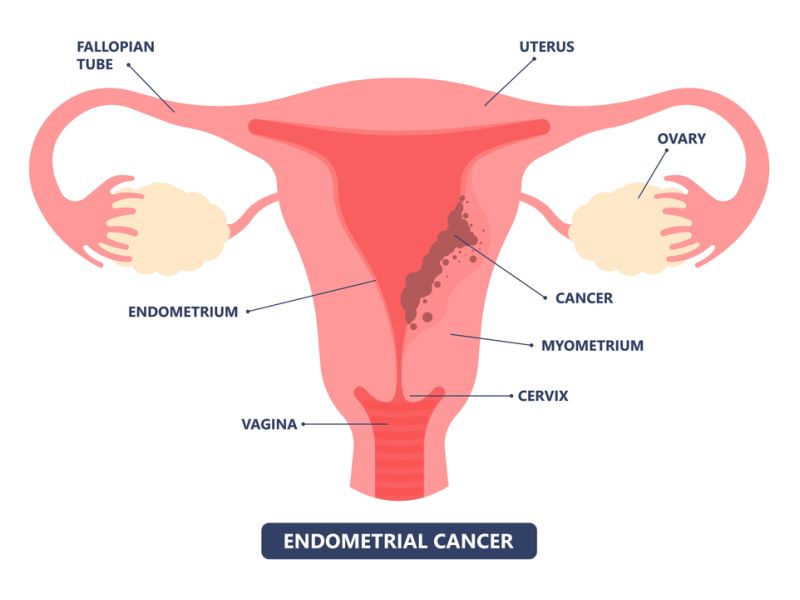
Endometrial cancer, often referred to as uterine cancer, is a kind of cancer that originates in the lining of the uterus, called the endometrium. It is one of the most common gynecologic malignancies, primarily affecting postmenopausal women, although it can occur in women of any age. Understanding the symptoms, stages, and treatments of endometrial cancer is vital for early detection & effective management of this condition.
The symptoms of endometrial cancer can vary, but the most common indicator is abnormal vaginal bleeding, particularly in postmenopausal women. This may include bleeding between periods or after menopause, as well as unusually heavy or prolonged menstrual periods. Additional symptoms may include pelvic pain, pain during intercourse, & abnormal vaginal discharge. It’s important for women to be aware of these signs and to promptly consult with a healthcare provider if they observe any concerning symptoms.
Treatment options for endometrial cancer depend on various factors, including the stage of the endometrial cancer, the patient’s overall health, & personal preferences. Surgery is the major treatment for most cases of endometrial cancer. It typically involves the removal of the uterus (hysterectomy) & often the fallopian tubes and ovaries as well (bilateral salpingo-oophorectomy). In certain cases, lymph nodes in the pelvis & abdomen may also be removed for staging purposes.
In addition to surgery, other treatment modalities may be recommended, such as radiation therapy, chemotherapy, hormone therapy, or targeted therapy. Radiation therapy (external beam radiation or brachytherapy) may be used to destroy cancer cells or reduce the risk of recurrence. Chemotherapy, hormone therapy, and targeted therapy are often employed in advanced or recurrent cases to target cancer cells and slow down disease progression.
Overall, the management of endometrial cancer requires a multidisciplinary approach involving gynecologic oncologists, radiation oncologists, medical oncologists, pathologists, and other healthcare professionals. Patient education, regular screening, and early detection are key to improving outcomes for individuals diagnosed with endometrial cancer. By raising awareness about the symptoms, stages, and treatment options, this blog aims to empower women with knowledge and encourage proactive healthcare-seeking behaviors.
Table of Contents
Endometrial Cancer Symptoms
Recognizing the symptoms of endometrial cancer is crucial for early detection and successful treatment. Here’s a detailed explanation of the symptoms:
1. Abnormal Vaginal Bleeding:
– The most common sign & symptom of endometrial cancer is unusual vaginal bleeding, particularly in postmenopausal women. This bleeding may include:
– Vaginal bleeding after menopause.
– Heavy or prolonged menstrual periods (menorrhagia).
– Bleeding between periods (metrorrhagia).
– Bleeding after intercourse (post-coital bleeding).
2. Pelvic Pain:
– Endometrial cancer may cause pelvic pain or discomfort, although this symptom is less common than abnormal vaginal bleeding.
– Pelvic pain may range from dull aches to sharp, intense pain.
– Pain may be localized to the pelvic area or may radiate to the lower abdomen or back.
3. Painful Urination:
– Some women with endometrial cancer may experience pain or discomfort during urination.
– This symptom can be due to the tumor pressing against the bladder or urethra.
4. Painful Intercourse:
– Endometrial cancer can cause pain during sexual intercourse (dyspareunia).
– This symptom may occur due to the presence of a tumor in the uterus or surrounding structures.
5. Pelvic Mass or Swelling:
– In advanced stages of uterine cancer, a pelvic mass or swelling may develop.
– The mass may be palpable during a pelvic examination or may be detected through imaging studies such as ultrasound or MRI.
6. Weight Loss and Fatigue:
– Unexplained weight loss and fatigue can be symptoms of advanced endometrial cancer.
– These symptoms may occur as a result of the body’s response to the cancer or due to the metabolic demands of the tumor.
7. Other Symptoms:
– Less commonly, endometrial cancer may cause symptoms such as bloating, constipation, or changes in bowel habits.
– These symptoms can occur if the tumor compresses or invades nearby structures such as the intestines.
It’s vital to note that these symptoms can also be caused by medical conditions other than endometrial cancer. However, any persistent or concerning symptoms should be evaluated by a healthcare professional. Early detection & treatment offer the best chance for successful outcomes in uterine cancer. Women experiencing any of these symptoms, especially postmenopausal bleeding, should seek medical attention promptly for further evaluation and diagnosis.
Endometrial Cancer Staging
Staging is a critical component in the treatment and prognosis of endometrial cancer. It refers to the extent of the disease and is determined after a thorough evaluation, which may include imaging tests and surgical procedures.
The most commonly used system for staging endometrial cancer is the FIGO system, which stands for the International Federation of Gynecology and Obstetrics. It classifies endometrial cancer into four main stages:
Stage I: The cancer is found only in the uterus.
Stage II: The cancer has metastasized from the uterus to the cervical stroma.
Stage III: The cancer has moved beyond the uterus but is still within the pelvic area.
Stage IV: Cancer has metastasized to distant body organs, such as the bladder, bowel, or lungs.
Each stage is further divided into sub-stages that provide more specific details about tumor size, lymph node involvement, and depth of invasion. Treatment decisions are based on the stage of cancer, with options ranging from surgery, radiation therapy, chemotherapy, hormone therapy, or a mixture of these treatments.
Early detection and accurate staging are essential for improving survival rates & quality of life for people with uterine cancer. Regular gynecological check-ups and reporting any unusual symptoms early can lead to timely diagnosis & treatment.
Endometrial Cancer Treatment
Treatment options vary based on the stage & grade of the cancer, & the patient’s overall health. In India, the cost of treatment can also be a significant factor for patients and their families. Here’s an overview of the common treatments and their approximate costs in India.
1. Surgery: Surgery, particularly hysterectomy, is the prevailing treatment for endometrial cancer. Depending on the stage of the disease, surgical procedures may entail the removal of both ovaries and fallopian tubes. The expenses for such surgeries typically range between INR 150,000 and INR 300,000.
2. Radiation Therapy: This treatment uses high-energy rays to kill cancer cells. It can be external beam radiation or brachytherapy (internal radiation). The price of radiation therapy can range from INR 1,00,000 to INR 2,50,000.
3. Chemotherapy: Chemotherapy involves using drugs to destroy cancer cells and may be given before or after surgery. The cost per cycle can vary widely from INR 50,000 to INR 2,00,000, depending on the drugs used.
4. Hormone Therapy: Hormone therapy may be an option if the cancer cells have hormone receptors. It can help slow or restrict the growth of cancer cells. Treatments can range from INR 10,000 to INR 50,000 per month.
5. Targeted Therapy: This type of treatment targets specific characteristics of cancer cells, like a protein that allows the cells to grow rapidly or abnormally. The costs are generally higher and can range from INR 1,00,000 to INR 4,00,000 per cycle.
6. Immunotherapy: A newer form of treatment that helps your immune system fight cancer. The costs for immunotherapy are quite high and can range from INR 1,00,000 to INR 5,00,000 per dose.
Please note that these costs are approximate and can differ based on several factors, including hospital choice, city, and patient-specific treatment plans.
Endometrial Cancer Causes
The exact cause of endometrial cancer isn’t fully understood, but various factors may contribute to its development:
1. Hormonal Factors: The most significant risk factor for endometrial cancer is exposure to estrogen without the counterbalancing effect of progesterone. Estrogen stimulates the development of the endometrium, while progesterone helps to counteract this growth. Factors that increase estrogen levels or decrease progesterone levels, such as hormone replacement therapy (HRT), obesity, early menstruation (before age 12), late menopause (after age 55), and polycystic ovary syndrome (PCOS), can increase the risk of endometrial cancer.
2. Obesity: Adipose tissue generates estrogen, and excess weight or obesity amplifies estrogen levels in the body, potentially fostering the development of uterine cancer.
3. Age: Endometrial cancer most commonly occurs in postmenopausal women, with the risk increasing with age.
4. Family History and Genetics: Having close relatives who have had endometrial or colorectal cancer increases the risk of developing uterine cancer. Certain hereditary conditions, such as Lynch syndrome (hereditary nonpolyposis colorectal cancer), which is driven by mutations in genes responsible for DNA repair, also raise the risk.
5. Endometrial Hyperplasia: This condition involves the abnormal thickening of the endometrium due to an excess of estrogen without enough progesterone. If left untreated, endometrial hyperplasia can advance to endometrial cancer.
6. Diabetes: Women with diabetes have an increased risk of endometrial cancer, possibly due to insulin resistance & higher levels of insulin in the body, which may promote the growth of endometrial cells.
7. Tamoxifen Therapy: Tamoxifen, a drug used in the treatment & prevention of breast cancer, has estrogen-like effects on the uterus and may slightly increase the risk of uterine cancer.
8. Reproductive Factors: Factors that affect a woman’s reproductive history, such as never having been pregnant, early menstruation, late menopause, or infertility, may increase the risk of endometrial cancer.
It’s essential to note that while these factors may increase the risk of endometrial cancer, having one or more risk factors doesn’t necessarily mean that someone will develop the disease. Additionally, many women diagnosed with uterine cancer do not have any identifiable risk factors. Regular screenings and awareness of symptoms can help with early detection and better treatment outcomes.
Endometrial Cancer Diagnosis
The diagnosis of endometrial cancer typically begins with a review of the patient’s medical history and a physical examination, including a pelvic exam. If there are symptoms suggestive of uterine cancer, such as abnormal vaginal bleeding or discharge, further tests may be recommended.
Diagnostic Tests:
1. Transvaginal Ultrasound: This test uses sound waves to create images of the uterus; it can help determine if the endometrium is abnormally thickened.
2. Endometrial Biopsy: A sample of endometrial tissue is collected and examined under a microscope for cancer cells.
3. Hysteroscopy: A thin, lighted tube is inserted into the uterus through the vagina to examine the endometrium and take tissue samples.
4. Dilation and Curettage (D&C): This procedure involves dilating the cervix and scraping tissue from the uterus’s lining for examination.
5. Imaging Tests: CT scans or MRIs may be used to determine if cancer has spread beyond the uterus.
If endometrial cancer is diagnosed, additional tests will be done to decide the stage of cancer, which guides treatment options. Staging may involve imaging tests like CT scans, MRIs, and sometimes PET scans to check for cancer spread.
What Is Endometrial Cancer?
Endometrial cancer originates in the endometrium, the lining of the uterus, and occurs when cells proliferate uncontrollably, forming a tumor. Predominantly impacting women, particularly post-menopause, it can also develop in younger individuals. Symptoms encompass irregular vaginal bleeding or discharge, pelvic discomfort, and pain during sexual intercourse. Timely detection and intervention are crucial for effectively addressing uterine cancer.
Endometrial Cancer Prognosis
Early detection plays an important role in the treatment success and survival rates. The five-year relative survival rates for endometrial cancer vary based on the stage of diagnosis:
– Localized (confined to the uterus): 95%
– Regional (spread to nearby areas): 70%
– Distant (spread to distant body organs): 18%
Overall, across all stages, the five-year relative survival rate averages around 81%. Factors such as age, overall health, and how well the cancer responds to treatment also influence an individual’s prognosis. It’s important to note that these statistics are based on data from women diagnosed and treated at least five years earlier. With advancements in medical treatments, women now being diagnosed with endometrial cancer (uterine cancer) may have a better outlook than these numbers suggest.
Conclusion
In conclusion, understanding the symptoms, stages, and treatment options for endometrial cancer is crucial for early detection and effective management. By staying informed, seeking timely medical attention, and exploring available treatments, individuals can improve their chances of favorable outcomes and quality of life. Ongoing research and advancements in care offer hope for continued progress in combating this significant health challenge.
Endometrial Cancer treatment often involves a combination of surgery, chemotherapy, & radiation therapy, which can be financially overwhelming for many individuals, particularly in a country like India, where healthcare expenses can be substantial. Crowdfunding provides a platform for patients to reach out to a larger community for financial assistance, easing the burden on them and their families.












