Chordoma is a rare type of cancer that develops from remnants of the notochord, a structure that forms in the early stages of fetal development and later becomes part of the spine. Although chordomas can occur anywhere along the spine, they most commonly affect the bones at the base of the skull and the lower end of the spine. This condition is characterised by slow-growing tumours that tend to invade nearby tissues and structures, making them challenging to treat.
Symptoms of chordoma can differ depending on the location and size of the tumour. Common symptoms include persistent back or neck pain, numbness in the arms or legs, problems while swallowing, headaches, and changes in bowel or bladder function. Because these symptoms can mimic those of other spinal conditions, diagnosis of chordoma may be delayed, leading to a more advanced stage of the disease at the time of diagnosis.
Life expectancy for individuals with chordoma can vary widely based on different factors, including the size & location of the tumour, how early it is diagnosed, and the effectiveness of treatment. While chordomas are typically slow-growing tumours, they can be locally aggressive, meaning they tend to invade surrounding tissues and structures. Additionally, chordomas have a high recurrence rate, even after surgery or radiation therapy.
Treatment options for chordoma typically involve a combination of surgery, radiation therapy, and sometimes chemotherapy. The goal of treatment is to remove as much of the tumour as possible while preserving neurological function and quality of life. However, because chordomas are located near critical structures such as the brainstem and spinal cord, complete surgical removal may not always be possible. In such cases, treatment may focus on relieving symptoms & slowing the progression of the disease.
Research into new treatments for chordoma is ongoing, with a particular focus on targeted therapies and immunotherapy. These approaches selectively target cancer cells while sparing healthy tissues, potentially offering more effective and less toxic treatment options for individuals with chordoma. Additionally, advances in imaging technology and surgical techniques continue to improve the ability to diagnose and treat chordomas accurately, leading to better outcomes for patients.
Table of Contents
Chordoma Symptoms
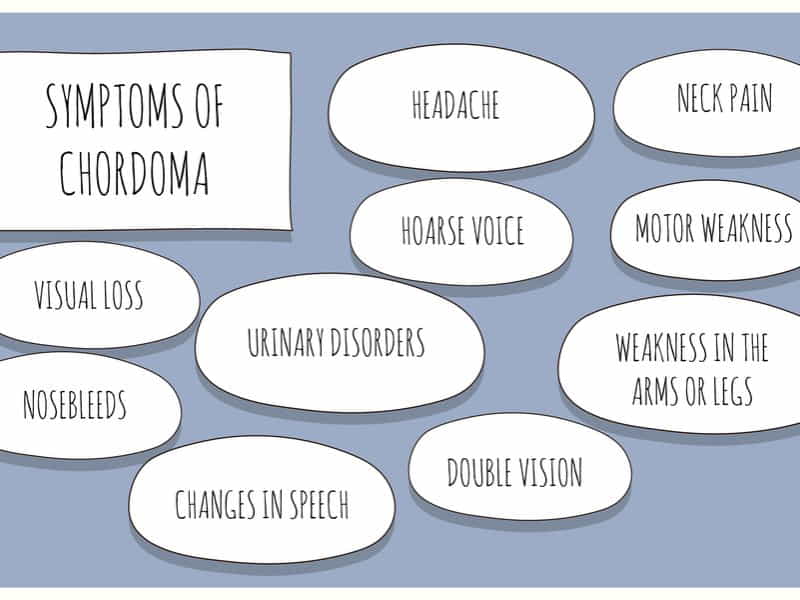
Chordomas usually grow slowly and may not cause symptoms for years. However, as they progress, they can lead to various symptoms due to their location and effects on surrounding tissues. Here’s a detailed explanation of the symptoms associated with chordoma:
1. Pain: Pain is one of the most common signs & symptoms of chordoma. The pain can be localised to the tumour site, typically in the skull base or spine. The pain may differ in intensity & can be described as dull, aching, or sharp. It may worsen with movement or pressure on the affected area.
2. Neurological Symptoms: Chordomas can compress nearby nerves or the spinal cord, causing neurological symptoms. These may include:
– Weakness: If the tumour compresses nerves that control muscle function, weakness may occur in the arms or legs.
– Numbness or Tingling: Compression of nerves can also cause numbness, tingling, or pins & needles in the arms, legs, or other body parts.
– Difficulty Walking: If the tumour affects the spinal cord, it can interfere with the normal function of walking, leading to difficulty in walking or maintaining balance.
– Changes in Bowel or Bladder Function: Severe spinal cord compression can affect the nerves controlling bowel and bladder function, leading to incontinence or difficulty with urination and bowel movements.
3. Headache: Chordomas located in the skull base can cause headaches, which may be persistent and worsen over time. These headaches are often dull and may be accompanied by other symptoms such as nausea or vomiting.
4. Visual Disturbances: Chordomas near the base of the skull can sometimes affect the nerves responsible for vision, leading to visual disturbances such as double vision or loss of peripheral vision.
5. Swelling or Mass: A noticeable swelling or mass may develop at the tumour site. This can sometimes be felt or seen as a lump, mainly if the tumour is located close to the body’s surface.
6. Difficulty Swallowing or Breathing: Chordomas located in the skull base can sometimes grow large enough to press on the structures of the throat or airway, leading to difficulty swallowing or breathing.
7. Other Symptoms: Depending on the specific location and size of the tumour, chordomas can cause various other symptoms, such as voice changes, hoarseness, ringing in the ears (tinnitus), or difficulty with balance and coordination.
It’s important to note that the symptoms of chordoma can vary widely depending on factors like the size & location of the tumour and individual differences in how the tumour affects nearby tissues and nerves. If you’re experiencing any persistent or concerning symptoms, it’s better to consult a medical professional for proper evaluation and diagnosis.
Chordoma Meaning
Chordoma is quite rare, meaning it doesn’t happen very often. It’s a type of cancer that typically shows up in bones, particularly in two specific areas: either along the spine or at the bottom of the skull.
To understand chordoma, we must go back to when a person is still an embryo. When we’re very tiny and still growing inside our mother’s womb, we have this structure called the notochord. This notochord is like a scaffold that helps shape our spine. As we develop, most notochord cells disappear or transform into other types of cells. However, in some cases, a few of these cells linger and stick around.
These lingering cells can turn into chordomas much later in life for reasons not entirely understood. Chordomas usually grow slowly, so they don’t spread quickly compared to other cancers. However, even though they’re slow-growing, they can still cause trouble. As they develop, they can put pressure on nearby nerves and tissues, leading to symptoms like back pain in the spine area or headaches near the skull base.
While chordoma is rare and can be challenging to treat, advancements in medical science have improved the chances of managing and even beating it.
Types Of Chordomas
Chordomas are rare, slow-growing tumours that usually occur along the spine, typically in the bones of the skull base and spine. There are three main types of chordomas based on their location:
1. Conventional chordoma: This type of chordoma is the most common and typically develops at the base of the skull or in the sacrum, the lower part of the spine.
2. Chondroid chordoma: These chordomas contain more cartilage-like tissue and are less aggressive than conventional chordomas.
3. Dedifferentiated chordoma: These aggressive tumours developed from a preexisting chordoma. They are often more difficult to treat and have a poorer prognosis than conventional chordomas.
Each type may require different treatment approaches and can have different prognoses.
Chordoma Life Expectancy
Understanding the survival rates of chordoma can provide insight into the prognosis and effectiveness of current treatments.
Globally, chordoma affects approximately one in one million people each year. The median age of diagnosis is in the 50s and 60s, with pediatric cases accounting for about 5% of all diagnoses. There is a slight gender variation in incidence, with males being more commonly diagnosed in adulthood.
Survival rates for chordoma vary depending on several factors, including the tumour’s location, the size, the patient’s age, and the treatments applied. Here are some general statistics on chordoma survival rates worldwide:
– The median overall survival for chordoma patients is reported to be 7.7 years, with a 5-year survival rate of 72%.
This rate drops to 48% at the 10-year mark and 31% at the 20-year mark.
– The prognosis for female patients is slightly better, with a median survival of 7.25 years compared to 5.93 years for male patients.
– The most recent 5-year relative survival rates based on diagnoses between 2011 and 2017 are as follows: 86% for localised chordoma (cancer has not spread), 85% for regional chordoma (cancer has spread into nearby structures, bones, or lymph nodes), and 61% for distant chordoma (cancer has metastasised to distant parts of the body).
Chordoma: Risk Factors and Causes
Chordoma is a rare kind of cancer that develops in the bones of the skull base & spine. It is a slow-growing yet malignant tumour that can have significant implications for those affected. Understanding chordoma’s risk factors and causes is crucial for early detection and treatment.
Risk Factors
The exact cause of chordoma is not fully known, but research has identified several factors that may increase the possibility of having this condition:
1. Age: Chordoma is most commonly diagnosed in adults between the ages of 40 & 70.
2. Gender: Men are almost twice as likely to develop chordoma as women.
3. Genetic Conditions: Some evidence suggests a genetic component to chordoma. For instance, people with a hereditary condition called tuberous sclerosis may have a higher incidence of developing chordoma.
Causes
Chordomas originate from notochord cells, which are embryonic cells that help form the spinal cord during prenatal development. In some cases, these cells can persist after birth and potentially develop into chordomas. The transformation of these notochord cells into cancerous tumours is not well understood, and currently, there is no known way to prevent it. However, several genetic factors have been associated with the development of chordoma.
Chordoma Treatment
In India, the treatment for chordoma typically involves a combination of surgery, radiation therapy, and, in some cases, chemotherapy. Here’s a detailed look at the treatment options available:
1. Surgery: Surgery is often the first choice of treatment for chordoma. The goal is to obliterate the tumour, which can be challenging due to the tumour’s proximity to critical structures like the spinal cord and brainstem. Advanced surgical techniques and experienced surgeons are required for the best outcomes.
2. Radiation Therapy: Post-surgical radiation therapy is commonly used to kill any remaining cancer cells. Techniques like proton beam therapy are preferred for their precision in targeting the tumour while sparing surrounding healthy tissue.
3. Chemotherapy: Chemotherapy is less commonly used for chordoma but may be considered if the tumour is aggressive or has metastasised. It involves utilising drugs to kill cancer cells.
4. Targeted Therapy: This is a newer area of treatment that involves drugs designed to target specific pathways that chordoma cells use to grow and divide.
5. Clinical Trials: Patients may also consider participating in clinical trials, which provide access to new therapies being tested for effectiveness.
The cost of treatment for chordoma in India varies widely based on the hospital’s location, the patient’s overall health, and the specific treatments required. On average, the cost starts at approximately USD 70 (around INR 5,600), but this is a very general estimate, and actual costs can be significantly higher, especially when considering advanced treatment options like proton beam therapy.
Please note that the costs mentioned are indicative and subject to change. It’s vital to consult with healthcare providers for the most accurate and current treatment costs.
How Are Chordomas Diagnosed?
The diagnosis of chordoma is a multi-step process that involves a combination of clinical evaluation, imaging, and histological analysis.
The initial suspicion of a chordoma often arises when a patient presents with pain, neurological deficits, or a palpable mass, depending on the tumour’s location. Given their slow growth and deep-seated nature, chordomas may not become symptomatic until they reach a considerable size, making early detection challenging.
Imaging techniques are vital in the diagnosis of chordomas. Magnetic Resonance Imaging (MRI) is typically the first-line imaging modality, providing detailed images of the tumour and its relationship with surrounding tissues. MRI can help determine the exact location of the cancer and whether it has invaded adjacent structures. Computed Tomography scans are also used to assess the extent of bone involvement and destruction caused by the tumour.
However, the definitive diagnosis of chordoma is made through histological examination. A biopsy is necessary to get a tissue sample of the tumour, which a pathologist examines under a microscope. The most common method is a needle biopsy, where a fine needle extracts a small amount of tissue from the tumour. This procedure is usually guided by imaging to ensure accuracy and minimise risk.
The microscopic analysis reveals the characteristic features of chordoma cells, which include physaliphorous cells – large cells with a bubbly appearance due to vacuoles containing mucin. Chordoma has three main histological subtypes: conventional (or classic), chondroid, and dedifferentiated, each with prognostic implications.
It’s important to note that chordomas are locally aggressive and can recur after treatment. In some cases, they may metastasise, spreading to other body parts such as the lungs, liver, or other bones. Therefore, accurate diagnosis is critical for effective management and treatment planning.
Conclusion
Chordoma is a rare type of cancer that affects the spine and skull base. While its symptoms can vary, they often include pain, numbness, and difficulty moving. Life expectancy can differ depending on factors like the tumour’s location and how early it’s diagnosed. Treatment options like surgery, radiation, & chemotherapy can help manage the condition. Overall, understanding chordoma’s meaning, symptoms, and treatment options is crucial for anyone facing this diagnosis.
Chordoma treatment can be costly, often including surgery, radiation therapy, and ongoing monitoring. Crowdfunding allows patients to reach out to a vast network of friends, family, and even strangers willing to contribute financially to their cause. It pools resources from multiple donors to help cover the hefty expenses associated with treatment.












